J Bone Metab.
2015 May;22(2):45-49. 10.11005/jbm.2015.22.2.45.
Result of Proficiency Test and Comparison of Accuracy Using a European Spine Phantom among the Three Bone Densitometries
- Affiliations
-
- 1Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Anesthesiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 4Division of Endocrinology and Metabolism, Sanbon Medical Center, University of Wonkwang College of Medicine, Iksan, Korea.
- 5Department of Nuclear Medicine, College of Medicine, Kyung Hee University, Seoul, Korea.
- 6Department of Orthopedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea. hayongch@naver.com
- KMID: 2170087
- DOI: http://doi.org/10.11005/jbm.2015.22.2.45
Abstract
- BACKGROUND
Although dual energy X-ray absorptiometry (DXA) is known to standard equipment for bone mineral density (BMD) measurements. Different results of BMD measurement using a number of different types of devices are difficult to use clinical practice. The purpose of this study was to evaluate discrepancy and standardizations of DXA devices from three manufactures using a European Spine Phantom (ESP).
METHODS
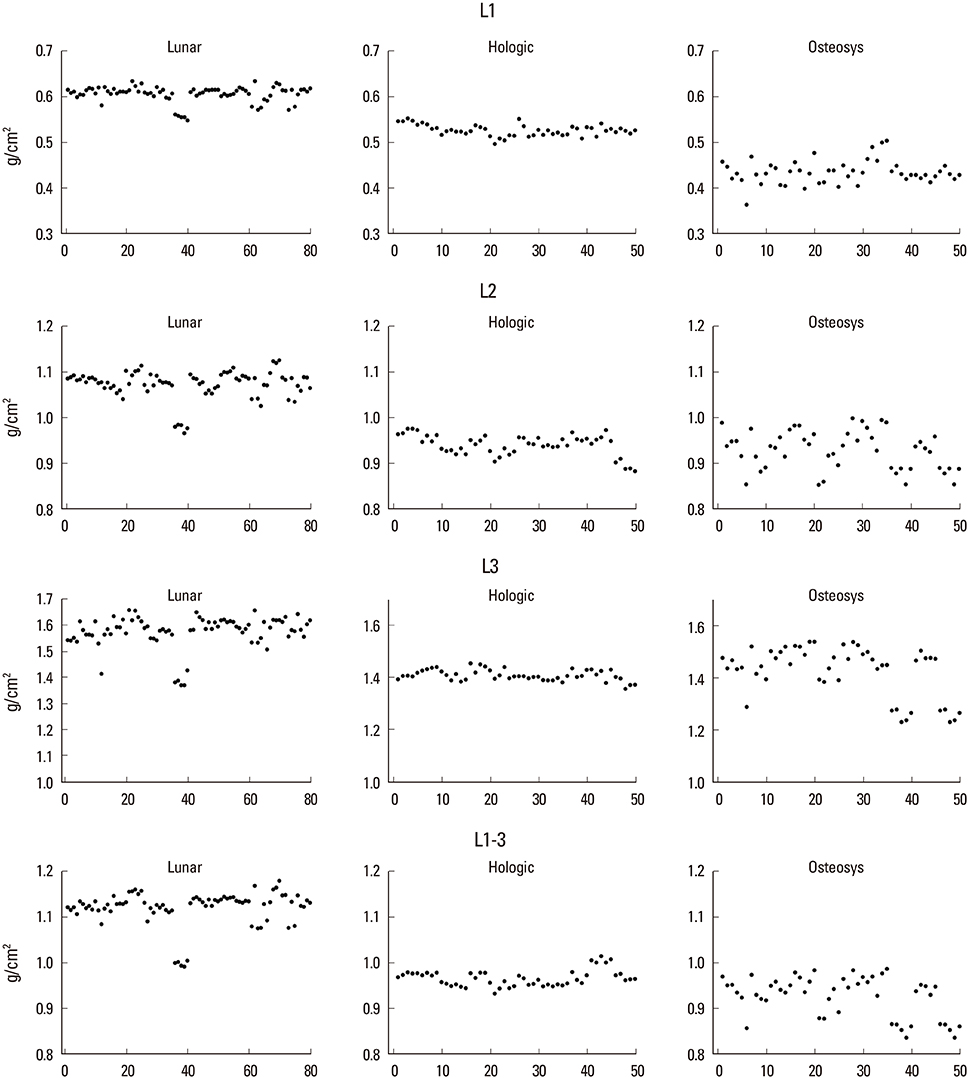
We calculated the accuracy and precision of 36 DXA devices from three manufacturers (10 Hologic, 16 Lunar, and 10 Osteosys) using a ESP (semi-anthropomorphic). The ESP was measured 5 times on each equipment without repositioning. Accuracy was assessed by comparing BMD (g/cm2) values measured on each device with the actual value of the phantom. Precision was assessed by the coefficient of variation (CVsd).
RESULTS
Lunar devices were, on average, 22%, 8.3%, and 5% overestimation for low (L1) BMD values, medium (L2), and high (L3) BMD values. Hologic devices were, on average, 6% overestimation for L1 BMD, and 5% and 6.2% underestimation for L2 and L3 BMD values. Osteosys devices was, on average, 12.7% (0.063 g/cm2), 6.3% (0.062 g/cm2), and 5% (0.075 g/cm2) underestimation for L1, L2, and L3, respectively. The mean CVsd for L1-L3 BMD were 0.01%, 0.78%, and 2.46% for Lunar, Hologic, and Osteosys devices respectively.
CONCLUSIONS
The BMD comparison in this study demonstrates that BMD result of three different devices are significant different between three devices. Differences of BMD between three devices are necessary to BMD standardization.
Figure
Cited by 1 articles
-
Measurement Uncertainty in Spine Bone Mineral Density by Dual Energy X-ray Absorptiometry
Ae-Ja Park, Jun-Il Yoo, Jee-Hye Choi, Kyun Shik Chae, Chang Geun Kim, Dal Sik Kim
J Bone Metab. 2017;24(2):105-109. doi: 10.11005/jbm.2017.24.2.105.
Reference
-
1. Genant HK, Cooper C, Poor G, et al. Interim report and recommendations of the World Health Organization Task-Force for Osteoporosis. Osteoporos Int. 1999; 10:259–264.
Article2. Genant HK, Grampp S, Gluer CC, et al. Universal standardization for dual x-ray absorptiometry: patient and phantom cross-calibration results. J Bone Miner Res. 1994; 9:1503–1514.
Article3. Pocock NA, Sambrook PN, Nguyen T, et al. Assessment of spinal and femoral bone density by dual X-ray absorptiometry: comparison of lunar and hologic instruments. J Bone Miner Res. 1992; 7:1081–1084.
Article4. Kolta S, Ravaud P, Fechtenbaum J, et al. Accuracy and precision of 62 bone densitometers using a European Spine Phantom. Osteoporos Int. 1999; 10:14–19.
Article5. Trevisan C, Gandolini GG, Sibilla P, et al. Bone mass measurement by DXA: influence of analysis procedures and interunit variation. J Bone Miner Res. 1992; 7:1373–1382.
Article6. Lees B, Garland SW, Walton C, et al. Evaluation of the European Spine Phantom in a multi-centre clinical trial. Osteoporos Int. 1997; 7:570–574.
Article7. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1:307–310.
Article8. Glüer CC, Blake G, Lu Y, et al. Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int. 1995; 5:262–270.
Article9. Mazess RB, Trempe JA, Bisek JP, et al. Calibration of dual-energy x-ray absorptiometry for bone density. J Bone Miner Res. 1991; 6:799–806.
Article10. Hui SL, Gao S, Zhou XH, et al. Universal standardization of bone density measurements: a method with optimal properties for calibration among several instruments. J Bone Miner Res. 1997; 12:1463–1470.
Article11. Ward KA, Ashby RL, Roberts SA, et al. UK reference data for the Hologic QDR Discovery dual-energy x ray absorptiometry scanner in healthy children and young adults aged 6-17 years. Arch Dis Child. 2007; 92:53–59.
Article12. Oldroyd B, Smith AH, Truscott JG. Cross-calibration of GE/Lunar pencil and fan-beam dual energy densitometers--bone mineral density and body composition studies. Eur J Clin Nutr. 2003; 57:977–987.
Article13. The Writing Group for the ISCD Position Development Conference. Technical standardization for dual-energy x-ray absorptiometry. J Clin Densitom. 2004; 7:27–36.14. Reid DM, Mackay I, Wilkinson S, et al. Cross-calibration of dual-energy X-ray densitometers for a large, multi-center genetic study of osteoporosis. Osteoporos Int. 2006; 17:125–132.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Phantoms to Protect Patients from Novices
- Measurement Uncertainty in Spine Bone Mineral Density by Dual Energy X-ray Absorptiometry
- Usefulness of ACR MRI Phantom for Quality Assurance of MRI Instruments
- In Vivo and In Vitro Studies of the Steady State Free Precession-Diffusion-Weighted MR Imagings on Low b-value: Validation and Application to Bone Marrow Pathology
- Enhancement of the Deformable Image Registration Accuracy Using Image Modification of MV CBCT