Anat Cell Biol.
2011 Mar;44(1):1-7. 10.5115/acb.2011.44.1.1.
Clinical and anatomical approach using Sihler's staining technique (whole mount nerve stain)
- Affiliations
-
- 1Division in Anatomy and Developmental Biology, Department of Oral Biology, Human Identification Research Center, College of Dentistry, Yonsei University, Seoul, Korea. hjk776@yuhs.ac
- 2Department of Oral Anatomy, Medical Research Institute, School of Dentistry, Pusan National University, Busan, Korea.
- KMID: 2168862
- DOI: http://doi.org/10.5115/acb.2011.44.1.1
Abstract
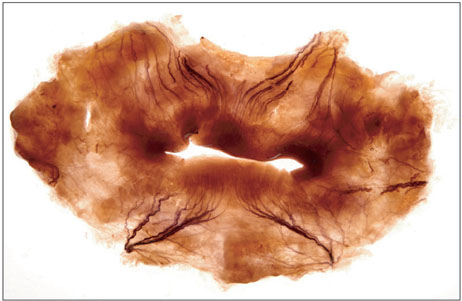
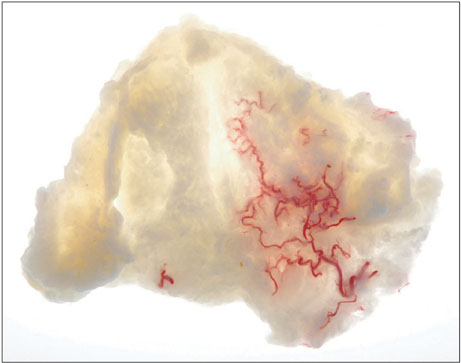
- Sihler's staining allows visualization of the nerve distribution within soft tissues without extensive dissection and does not require slide preparation, unlike traditional approaches. This technique can be applied to the mucosa, muscle, and organs that contain myelinated nerve fibers. In particular, Sihler's technique may be considered the best tool for observing nerve distribution within skeletal muscles. The intramuscular distribution pattern of nerves is difficult to observe through manual manipulation due to the gradual tapering of nerves toward the terminal end of muscles, so it should be accompanied by histological studies to establish the finer branches therein. This method provides useful information not only for anatomists but also for physiologists and clinicians. Advanced knowledge of the nerve distribution patterns will be useful for developing guidelines for clinicians who perform operations such as muscle resection, tendon transplantation, and botulinum toxin injection. Furthermore, it is a useful technique to develop neurosurgical techniques and perform electrophysiological experiments. In this review, Sihler's staining technique is described in detail, covering its history, staining protocol, advantages, disadvantages, and possible applications. The application of this technique for determining the arterial distribution pattern is also described additionally in this study.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Morphology of the temporalis muscle focusing on the tendinous attachment onto the coronoid process
Sun Kyoung Yu, Tae-Hoon Kim, Kwang Yeol Yang, Christopher J. Bae, Heung-Joong Kim
Anat Cell Biol. 2021;54(3):308-314. doi: 10.5115/acb.21.074.
Reference
-
1. Sihler C. Ueber muskelspindeln und intramuskuläre nervenendigungen bei schlangen und röschen. Arch Mikrosk Anat. 1895. 46:709–723.2. Sihler C. Die Muskelspindeln Kerne und Lage der motorischen Nervenendigungen Zugleich em Nachtrag zu der Arbeit: Ueber Muskelspindeln etc Dieses Archiv Bd. XXXXVI, pg. 709. Archiv Mikrosk Anat. 1900. 56:334–354.3. Wharton LR. A technique for studying the innervation of organs. Anat Rec. 1937. 67:469–475.4. Williams TW Jr. A technique for the gross differential staining of peripheral nerves in cleared vertebrate tissue. Anat Rec. 1943. 86:189–195.5. Freihofer WC. The Sihler technique of staining nerves for systematic study especially of fishes. Copeia. 1966. 3:470–475.6. Liem RS, Douwe van Willigen J. In toto staining and preservation of peripheral nervous tissue. Stain Technol. 1988. 63:113–120.7. Wu BL, Sanders I. A technique for demonstrating the nerve supply of whole larynges. Arch Otolaryngol Head Neck Surg. 1992. 118:822–827.8. Sanders I, Wu BL, Mu L, Li Y, Biller HF. The innervation of the human larynx. Arch Otolaryngol Head Neck Surg. 1993. 119:934–939.9. Sanders I, Wu BL, Mu L, Biller HF. The innervation of the human posterior cricoarytenoid muscle: evidence for at least two neuromuscular compartments. Laryngoscope. 1994. 104:880–884.10. Mu L, Sanders I. The innervation of the human upper esophageal sphincter. Dysphagia. 1996. 11:234–238.11. Mu L, Sanders I. Neuromuscular organization of the human upper esophageal sphincter. Ann Otol Rhinol Laryngol. 1998. 107(5 Pt 1):370–377.12. Mu L, Sanders I. Neuromuscular organization of the canine tongue. Anat Rec. 1999. 256:412–424.13. Kim DH, Hong HS, Won SY, Kim HJ, Hu KS, Choi JH, Kim HJ. Intramuscular nerve distribution of the masseter muscle as a basis for botulinum toxin injection. J Craniofac Surg. 2010. 21:588–591.14. Maeda S, Miyawaki T, Kuboki T, Shimada M. A trigeminal neuralgia-like paroxysmal pain condition presumably due to buccal nerve compression in the temporalis muscle. Cranio. 2001. 19:56–60.15. Touré G, Bicchieray L, Selva J, Vacher C. The intra-lingual course of the nerves of the tongue. Surg Radiol Anat. 2005. 27:297–302.16. Gurney CE. Chronic bilateral benign hypertrophy of the masseter muscles. Am J Surg. 1947. 73:137–139.17. Park MY, Ahn KY, Jung DS. Botulinum toxin type A treatment for contouring of the lower face. Dermatol Surg. 2003. 29:477–483.18. Kim NH, Chung JH, Park RH, Park JB. The use of botulinum toxin type A in aesthetic mandibular contouring. Plast Reconstr Surg. 2005. 115:919–930.19. Lepage D, Parratte B, Tatu L, Vuiller F, Monnier G. Extra- and intramuscular nerve supply of the muscles of the anterior antebrachial compartment: applications for selective neurotomy and for botulinum toxin injection. Surg Radiol Anat. 2005. 27:420–430.20. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 2005. 39th ed. New York: Churchill Livingstone;520–521.21. Won SY, Hur MS, Rha DW, Park HD, Hu KS, Fontaine C, Kim HJ. Extra- and intramuscular nerve distribution patterns of the muscles of the ventral compartment of the forearm. Am J Phys Med Rehabil. 2010. 89:644–652.22. Park ES, Rha DW. Botulinum toxin type A injection for management of upper limb spasticity in children with cerebral palsy: a literature review. Yonsei Med J. 2006. 47:589–603.23. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 2005. 39th ed. New York: Churchill Livingstone;1467–1468.24. Ofluoglu D, Esquenazi A, Hirai B. Temporospatial parameters of gait after obturator neurolysis in patients with spasticity. Am J Phys Med Rehabil. 2003. 82:832–836.25. Kwon JY, Kim JS, Lee WI. Anatomic localization of motor points of hip adductors. Am J Phys Med Rehabil. 2009. 88:336–341.26. Childers MK. Targeting the neuromuscular junction in skeletal muscles. Am J Phys Med Rehabil. 2004. 83:10 Suppl. S38–S44.27. Christensen E. Topography of terminal motor innervation in striated muscles from stillborn infants. Am J Phys Med. 1959. 38:65–78.28. Crystal R, Malone AA, Eastwood DM. Motor points for neuromuscular blockade of the adductor muscle group. Clin Orthop Relat Res. 2005. (437):196–200.29. Van Campenhout A, Molenaers G. Localization of the motor endplate zone in human skeletal muscles of the lower limb: anatomical guidelines for injection with botulinum toxin. Dev Med Child Neurol. 2011. 53:108–119.30. Van Campenhout A, Hubens G, Fagard K, Molenaers G. Localization of motor nerve branches of the human psoas muscle. Muscle Nerve. 2010. 42:202–207.31. Kim SC, Kang MH, Ock JJ. Calf-contouring surgery of gastrocnemius hypertrophy: selective neurectomy of the sural nerve. Aesthetic Plast Surg. 2008. 32:889–893.32. Tsai FC, Mardini S, Fong TH, Kang JH, Chou CM. Selective neurectomy of the gastrocnemius and soleus muscles for calf hypertrophy: an anatomical study and 700 clinical cases. Plast Reconstr Surg. 2008. 122:178–187.33. Lemperle G, Exner K. The resection of gastrocnemius muscles in aesthetically disturbing calf hypertrophy. Plast Reconstr Surg. 1998. 102:2230–2236.34. Han KH, Joo YH, Moon SE, Kim KH. Botulinum toxin A treatment for contouring of the lower leg. J Dermatolog Treat. 2006. 17:250–254.35. Yoo WK, Chung IH, Park CI. Anatomic motor point localization for the treatment of gastrocnemius muscle spasticity. Yonsei Med J. 2002. 43:627–630.36. Liu J, Kumar VP, Shen Y, Lau HK, Pereira BP, Pho RW. Modified Sihler's technique for studying the distribution of intramuscular nerve branches in mammalian skeletal muscle. Anat Rec. 1997. 247:137–144.37. Sheverdin VA, Hur MS, Won SY, Song WC, Hu KS, Koh KS, Kim HJ. Extra- and intramuscular nerves distributions of the triceps surae muscle as a basis for muscle resection and botulinum toxin injections. Surg Radiol Anat. 2009. 31:615–621.38. Dominiak M, Konopka T. Gingival esthetics in periodontology. E-Dentico. 2005. (2):6–15.39. Reiser GM, Bruno JF, Mahan PE, Larkin LH. The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 1996. 16:130–137.40. Cordioli G, Mortarino C, Chierico A, Grusovin MG, Majzoub Z. Comparison of 2 techniques of subepithelial connective tissue graft in the treatment of gingival recessions. J Periodontol. 2001. 72:1470–1476.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CONSERVATIVE PAROTIDECTOMY BY THE ANTERIOR APPROACH
- Anatomical study of the nerve regeneration after selective neurectomy in the rabbit: clinical application for esthetic calf reduction
- The Effect of Melatonin Injection into Rat Brain Stem with Chronic Stress on Serotonergic Immunoreactivity
- Facial Nerve Paralysis and Surgical Management
- Comparative Assessment of Immunohistochemical and Zieh1-Neelsen Stains for Demonstration of Mycobacterium Tuberculosis