Cancer Res Treat.
2013 Dec;45(4):295-302.
Predictive Factors for Radiation Pneumonitis in Lung Cancer Treated with Helical Tomotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Kyung Hee University Medical Center, Kyung Hee University School of Medicine, Seoul, Korea. kongmoonkyoo@khu.ac.kr
Abstract
- PURPOSE
Predictive factors for radiation pneumonitis (RP) after helical tomotherapy (HT) may differ from those after linac-based radiotherapy. In this study, we identified predictive factors for RP in patients with lung cancer treated with HT.
MATERIALS AND METHODS
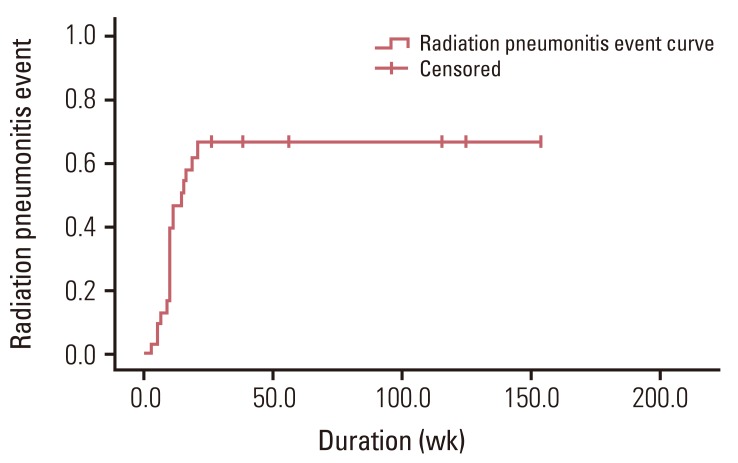
We retrospectively analyzed clinical, treatment-related and dosimetric factors from 31 patients with lung cancer treated with HT. RP was graded according to Common Terminology Criteria for Adverse Events version 4.0 and grade > or =2 RP was defined as a RP event. We used Kaplan-Meier methods to compute the actuarial incidence of RP. For univariate and multivariate analysis, the log-rank test and the Cox proportional regression hazard model were used. We generated receiver-operating characteristics (ROC) curves to define the cutoff values for significant parameters.
RESULTS
The median follow-up duration was 6.6 months (range, 1.6 to 38.5 months). The 2-, 4-, and 6-month actuarial RP event rates were 13.2%, 58.5%, and 67.0%, respectively. There was no grade 4 or more RP. Ipsilateral V5, V10, V15, and contralateral V5 were related with RP event on univariate analysis. By multivariate analysis, ipsilateral V10 was factor most strongly associated with RP event. On the ROC curve, the cutoff values of ipsilateral V5, V10, V15, and contralateral V5 were 67.5%, 58.5%, 50.0%, and 55.5%, respectively.
CONCLUSION
In our study, ipsilateral V5, V10, V15, and contralateral V5 were significant predictive factors for RP after HT.
MeSH Terms
Figure
Reference
-
1. Clenton SJ, Fisher PM, Conway J, Kirkbride P, Hatton MQ. The use of lung dose-volume histograms in predicting post-radiation pneumonitis after non-conventionally fractionated radiotherapy for thoracic carcinoma. Clin Oncol (R Coll Radiol). 2005; 17:599–603. PMID: 16372484.
Article2. Fay M, Tan A, Fisher R, Mac Manus M, Wirth A, Ball D. Dose-volume histogram analysis as predictor of radiation pneumonitis in primary lung cancer patients treated with radiotherapy. Int J Radiat Oncol Biol Phys. 2005; 61:1355–1363. PMID: 15817337.
Article3. Hernando ML, Marks LB, Bentel GC, Zhou SM, Hollis D, Das SK, et al. Radiation-induced pulmonary toxicity: a dose-volume histogram analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol Phys. 2001; 51:650–659. PMID: 11597805.
Article4. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005; 235:208–215. PMID: 15703313.
Article5. Kim M, Lee J, Ha B, Lee R, Lee KJ, Suh HS. Factors predicting radiation pneumonitis in locally advanced non-small cell lung cancer. Radiat Oncol J. 2011; 29:181–190. PMID: 22984669.
Article6. Yom SS, Liao Z, Liu HH, Tucker SL, Hu CS, Wei X, et al. Initial evaluation of treatment-related pneumonitis in advanced-stage non-small-cell lung cancer patients treated with concurrent chemotherapy and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:94–102. PMID: 17321067.
Article7. Tsujino K, Hirota S, Kotani Y, Kado T, Yoden E, Fujii O, et al. Radiation pneumonitis following concurrent accelerated hyperfractionated radiotherapy and chemotherapy for limited-stage small-cell lung cancer: Dose-volume histogram analysis and comparison with conventional chemoradiation. Int J Radiat Oncol Biol Phys. 2006; 64:1100–1105. PMID: 16373082.
Article8. Wang S, Liao Z, Wei X, Liu HH, Tucker SL, Hu CS, et al. Analysis of clinical and dosimetric factors associated with treatment-related pneumonitis (TRP) in patients with non-small-cell lung cancer (NSCLC) treated with concurrent chemotherapy and three-dimensional conformal radiotherapy (3D-CRT). Int J Radiat Oncol Biol Phys. 2006; 66:1399–1407. PMID: 16997503.
Article9. Rancati T, Ceresoli GL, Gagliardi G, Schipani S, Cattaneo GM. Factors predicting radiation pneumonitis in lung cancer patients: a retrospective study. Radiother Oncol. 2003; 67:275–283. PMID: 12865175.
Article10. Rodrigues GB. A prospective study on radiation pneumonitis following conformal radiation therapy in non-small-cell lung cancer: clinical and dosimetric factors analysis. Radiother Oncol. 2005; 75:120–121. PMID: 15878110.11. Mackie TR, Holmes T, Swerdloff S, Reckwerdt P, Deasy JO, Yang J, et al. Tomotherapy: a new concept for the delivery of dynamic conformal radiotherapy. Med Phys. 1993; 20:1709–1719. PMID: 8309444.
Article12. Scrimger RA, Tome WA, Olivera GH, Reckwerdt PJ, Mehta MP, Fowler JF. Reduction in radiation dose to lung and other normal tissues using helical tomotherapy to treat lung cancer, in comparison to conventional field arrangements. Am J Clin Oncol. 2003; 26:70–78. PMID: 12576928.
Article13. Cattaneo GM, Dell'oca I, Broggi S, Fiorino C, Perna L, Pasetti M, et al. Treatment planning comparison between conformal radiotherapy and helical tomotherapy in the case of locally advanced-stage NSCLC. Radiother Oncol. 2008; 88:310–318. PMID: 18692266.
Article14. Kron T, Grigorov G, Yu E, Yartsev S, Chen JZ, Wong E, et al. Planning evaluation of radiotherapy for complex lung cancer cases using helical tomotherapy. Phys Med Biol. 2004; 49:3675–3690. PMID: 15446797.
Article15. Song CH, Pyo H, Moon SH, Kim TH, Kim DW, Cho KH. Treatment-related pneumonitis and acute esophagitis in non-small-cell lung cancer patients treated with chemotherapy and helical tomotherapy. Int J Radiat Oncol Biol Phys. 2010; 78:651–658. PMID: 20207499.
Article16. Giraud P, Antoine M, Larrouy A, Milleron B, Callard P, De Rycke Y, et al. Evaluation of microscopic tumor extension in non-small-cell lung cancer for three-dimensional conformal radiotherapy planning. Int J Radiat Oncol Biol Phys. 2000; 48:1015–1024. PMID: 11072158.
Article17. Jiang ZQ, Yang K, Komaki R, Wei X, Tucker SL, Zhuang Y, et al. Long-term clinical outcome of intensity-modulated radiotherapy for inoperable non-small cell lung cancer: the MD Anderson experience. Int J Radiat Oncol Biol Phys. 2012; 83:332–339. PMID: 22079735.
Article18. Yamada M, Kudoh S, Hirata K, Nakajima T, Yoshikawa J. Risk factors of pneumonitis following chemoradiotherapy for lung cancer. Eur J Cancer. 1998; 34:71–75. PMID: 9624240.
Article19. Byhardt RW, Scott C, Sause WT, Emami B, Komaki R, Fisher B, et al. Response, toxicity, failure patterns, and survival in five Radiation Therapy Oncology Group (RTOG) trials of sequential and/or concurrent chemotherapy and radiotherapy for locally advanced non-small-cell carcinoma of the lung. Int J Radiat Oncol Biol Phys. 1998; 42:469–478. PMID: 9806503.
Article20. Seppenwoolde Y, Lebesque JV, de Jaeger K, Belderbos JS, Boersma LJ, Schilstra C, et al. Comparing different NTCP models that predict the incidence of radiation pneumonitis. Normal tissue complication probability. Int J Radiat Oncol Biol Phys. 2003; 55:724–735. PMID: 12573760.21. Yorke ED, Jackson A, Rosenzweig KE, Braban L, Leibel SA, Ling CC. Correlation of dosimetric factors and radiation pneumonitis for non-small-cell lung cancer patients in a recently completed dose escalation study. Int J Radiat Oncol Biol Phys. 2005; 63:672–682. PMID: 15939548.
Article22. Oh D, Ahn YC, Park HC, Lim do H, Han Y. Prediction of radiation pneumonitis following high-dose thoracic radiation therapy by 3 Gy/fraction for non-small cell lung cancer: analysis of clinical and dosimetric factors. Jpn J Clin Oncol. 2009; 39:151–157. PMID: 19193653.
Article23. Roach M 3rd, Gandara DR, Yuo HS, Swift PS, Kroll S, Shrieve DC, et al. Radiation pneumonitis following combined modality therapy for lung cancer: analysis of prognostic factors. J Clin Oncol. 1995; 13:2606–2612. PMID: 7595714.
Article24. Robnett TJ, Machtay M, Vines EF, McKenna MG, Algazy KM, McKenna WG. Factors predicting severe radiation pneumonitis in patients receiving definitive chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys. 2000; 48:89–94. PMID: 10924976.
Article25. Shi A, Zhu G, Wu H, Yu R, Li F, Xu B. Analysis of clinical and dosimetric factors associated with severe acute radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with concurrent chemotherapy and intensity-modulated radiotherapy. Radiat Oncol. 2010; 5:35. PMID: 20462424.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of survival rates between patients treated with conventional radiotherapy and helical tomotherapy for head and neck cancer
- Helical Tomotherapy: Image-guided Intensity Modulated Radiation Therapy
- Radiation Induced Lung Damage : Mechanisms and Clinical Implications
- The Studies on the Development of Radiation Pneumonitis and Its Related Factors
- Bilateral Diffuse Radiation Pneumonitis Caused by Unilateral Thoracic Irradiation: A Case Report