Cancer Res Treat.
2013 Mar;45(1):55-62.
Impact of KRAS Mutation Status on Outcomes in Metastatic Colon Cancer Patients without Anti-Epidermal Growth Factor Receptor Therapy
- Affiliations
-
- 1Division of Hematology-Oncology, Department of Medicine, Korea University College of Medicine, Seoul, Korea. yhk0215@korea.ac.kr
Abstract
- PURPOSE
Activating mutation of the KRAS oncogene is an established negative predictor for anti-epidermal growth factor receptor (anti-EGFR) therapies in metastatic colorectal cancer (CRC). However, KRAS mutation as a prognostic factor of survival outcome remains controversial in CRC, independent of anti-EGFR therapies.
MATERIALS AND METHODS
We conducted a retrospective analysis of 103 CRC patients who were available for evaluation of KRAS mutation status. None of the patients analyzed had received anti-EGFR therapies. The role of KRAS mutation status was evaluated as a predictive factor for oxaliplatin or irinotecan and as a prognostic factor in CRC patients who did not receive anti-EGFR therapies.
RESULTS
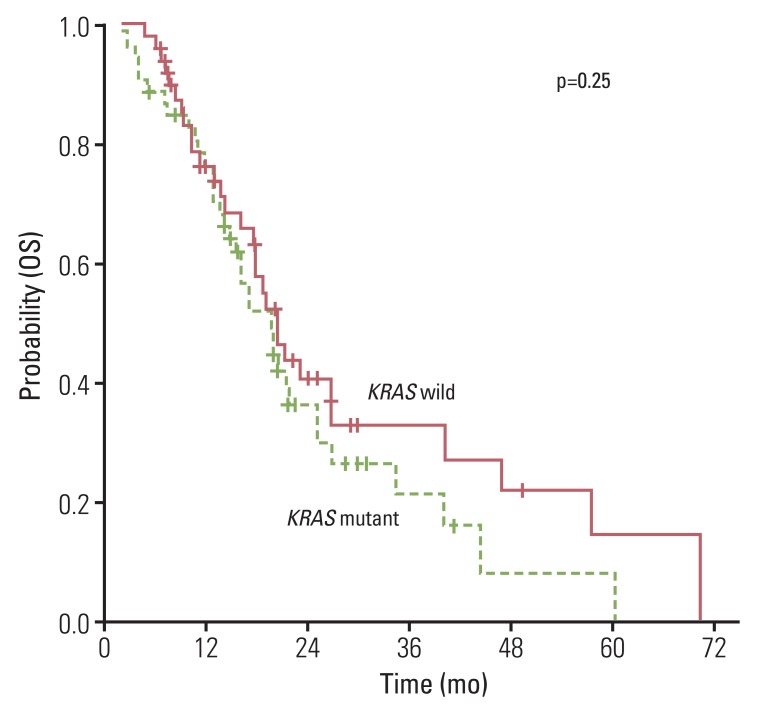
Mutations in KRAS were observed in 48.5% of patients. The response for oxaliplatin- (p=0.664) and irinotecan-based (p=0.255) cytotoxic chemotherapy did not differ according to the KRAS mutation status. In addition, no significant difference in progression free survival (PFS; oxaliplatin, p=0.583 and irinotecan, p=0.426) and overall survival (OS; p=0.258) was observed between the wild and mutant type of the KRAS gene. In univariate and multivariate analyses, KRAS mutations did not have a major prognostic value regarding PFS (oxaliplatin: hazard ratio, 0.892; 95% confidence interval [CI], 0.590 to 1.347; p=0.586 and irinotecan: hazard ratio, 0.831; 95% CI, 0.524 to 1.319; p=0.433) or OS (hazard ratio, 0.754; 95% CI, 0.460 to 1.236; p=0.263). In addition, anti-vascular endothelial growth factor therapies did not affect PFS to oxaliplatin or irinotecan and OS.
CONCLUSION
KRAS mutation is not a prognostic marker for PFS to oxaliplatin or irinotecan and OS in CRC patients who did not receive anti-EGFR therapies.
Keyword
MeSH Terms
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108. PMID: 15761078.
Article2. de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000; 18:2938–2947. PMID: 10944126.
Article3. Saltz LB, Cox JV, Blanke C, Rosen LS, Fehrenbacher L, Moore MJ, et al. Irinotecan Study Group. Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. N Engl J Med. 2000; 343:905–914. PMID: 11006366.
Article4. Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988; 319:525–532. PMID: 2841597.
Article5. Hamelin R, Laurent-Puig P, Olschwang S, Jego N, Asselain B, Remvikos Y, et al. Association of p53 mutations with short survival in colorectal cancer. Gastroenterology. 1994; 106:42–48. PMID: 8276207.
Article6. Ahnen DJ, Feigl P, Quan G, Fenoglio-Preiser C, Lovato LC, Bunn PA Jr, et al. Ki-ras mutation and p53 overexpression predict the clinical behavior of colorectal cancer: a Southwest Oncology Group study. Cancer Res. 1998; 58:1149–1158. PMID: 9515799.7. Schubbert S, Shannon K, Bollag G. Hyperactive Ras in developmental disorders and cancer. Nat Rev Cancer. 2007; 7:295–308. PMID: 17384584.
Article8. Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008; 26:1626–1634. PMID: 18316791.9. Karapetis CS, Khambata-Ford S, Jonker DJ, O'Callaghan CJ, Tu D, Tebbutt NC, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008; 359:1757–1765. PMID: 18946061.10. Klump B, Nehls O, Okech T, Hsieh CJ, Gaco V, Gittinger FS, et al. Molecular lesions in colorectal cancer: impact on prognosis? Original data and review of the literature. Int J Colorectal Dis. 2004; 19:23–42. PMID: 12827409.11. Roth AD, Tejpar S, Delorenzi M, Yan P, Fiocca R, Klingbiel D, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol. 2010; 28:466–474. PMID: 20008640.
Article12. Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML. Relationship of Ki-ras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomarkers Prev. 2000; 9:1193–1197. PMID: 11097226.13. Ince WL, Jubb AM, Holden SN, Holmgren EB, Tobin P, Sridhar M, et al. Association of k-ras, b-raf, and p53 status with the treatment effect of bevacizumab. J Natl Cancer Inst. 2005; 97:981–989. PMID: 15998951.
Article14. Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009; 360:1408–1417. PMID: 19339720.
Article15. Anwar S, Frayling IM, Scott NA, Carlson GL. Systematic review of genetic influences on the prognosis of colorectal cancer. Br J Surg. 2004; 91:1275–1291. PMID: 15382104.
Article16. Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006; 24:5313–5327. PMID: 17060676.
Article17. Gonzalez-Aguilera JJ, Oliart S, Azcoita MM, Fernandez-Peralta AM. Simultaneous mutations in K-ras and TP53 are indicative of poor prognosis in sporadic colorectal cancer. Am J Clin Oncol. 2004; 27:39–45. PMID: 14758132.18. Westra JL, Schaapveld M, Hollema H, de Boer JP, Kraak MM, de Jong D, et al. Determination of TP53 mutation is more relevant than microsatellite instability status for the prediction of disease-free survival in adjuvant-treated stage III colon cancer patients. J Clin Oncol. 2005; 23:5635–5643. PMID: 16110022.
Article19. Andreyev HJ, Norman AR, Cunningham D, Oates JR, Clarke PA. Kirsten ras mutations in patients with colorectal cancer: the multicenter "RASCAL" study. J Natl Cancer Inst. 1998; 90:675–684. PMID: 9586664.
Article20. Andreyev HJ, Norman AR, Cunningham D, Oates J, Dix BR, Iacopetta BJ, et al. Kirsten ras mutations in patients with colorectal cancer: the 'RASCAL II' study. Br J Cancer. 2001; 85:692–696. PMID: 11531254.21. Leslie A, Pratt NR, Gillespie K, Sales M, Kernohan NM, Smith G, et al. Mutations of APC, K-ras, and p53 are associated with specific chromosomal aberrations in colorectal adenocarcinomas. Cancer Res. 2003; 63:4656–4661. PMID: 12907646.22. Baker SJ, Preisinger AC, Jessup JM, Paraskeva C, Markowitz S, Willson JK, et al. p53 gene mutations occur in combination with 17p allelic deletions as late events in colorectal tumorigenesis. Cancer Res. 1990; 50:7717–7722. PMID: 2253215.23. Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990; 61:759–767. PMID: 2188735.
Article24. Richman SD, Seymour MT, Chambers P, Elliott F, Daly CL, Meade AM, et al. KRAS and BRAF mutations in advanced colorectal cancer are associated with poor prognosis but do not preclude benefit from oxaliplatin or irinotecan: results from the MRC FOCUS trial. J Clin Oncol. 2009; 27:5931–5937. PMID: 19884549.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dose KRAS Mutation Status Affect on the Effect of VEGF Therapy in Metastatic Colon Cancer Patients?
- Amplification of epidermal growth factor receptor gene in primary cervical cancer
- Amplification of epidermal growth factor receptor gene in primary cervical cancer
- Prognostic significance of epidermal growth factor receptor expression in human gastric carcinoma
- Epidermal Growth Factor Receptor Mutation Status in the Treatment of Non-small Cell Lung Cancer: Lessons Learned