Cancer Res Treat.
2011 Sep;43(3):176-180.
The Usefulness of Procalcitonin and C-Reactive Protein as Early Diagnostic Markers of Bacteremia in Cancer Patients with Febrile Neutropenia
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ysdoc@amc.seoul.kr
Abstract
- PURPOSE
Procalcitonin (PCT) and C-reactive protein (CRP) are well known inflammatory markers. This study was designed to determine whether PCT and CRP are useful as early diagnostic markers for bacteremia in cancer patients with febrile neutropenia (FN) in the emergency department (ED).
MATERIALS AND METHODS
In this retrospective study, 286 episodes of FN in the ED were consecutively included between June 2009 and August 2010. From medical records, clinical characteristics including PCT and CRP were extracted and analyzed.
RESULTS
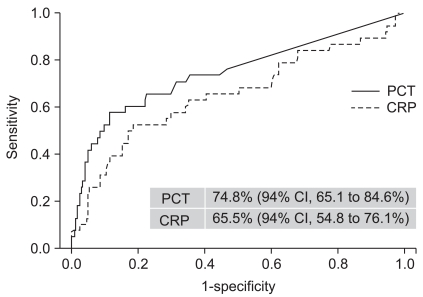
Bacteremia was identified in 38 (13.3%) of the 286 episodes. The median values of PCT (2.8 ng/mL vs. 0.0 ng/mL, p=0.000) and CRP (15.9 mg/dL vs. 5.6 mg/dL, p=0.002) were significantly higher in the group with bacteremia compared to the group without bacteremia. In univariate analysis, elevated PCT (>0.5 ng/mL) and CRP (>10 mg/dL) as well as older age, hypotension, tachycardia, tachypnea, and high body temperature were significantly associated with bacteremia. On multivariate analysis, elevated PCT (>0.5 ng/mL) (odds ratio [OR], 3.6; 95% confidence interval [CI], 1.4 to 9.2; p<0.01) and tachypnea (OR, 3.4; 95% CI, 1.4 to 8.5; p<0.01) were independent early diagnostic markers for bacteremia in FN patients. The area under the curve of PCT was 74.8% (95% CI, 65.1 to 84.6%) and that of CRP was 65.5% (95% CI, 54.8 to 76.1%). With a PCT cut-off value of 0.5 ng/mL, sensitivity and specificity were 60.5% and 82.3%, respectively, while the sensitivity and specificity were 57.6% and 67.3%, respectively, with a CRP cutoff of 10 mg/dL.
CONCLUSION
These findings suggest that PCT is a useful early diagnostic marker for the detection of bacteremia in FN at the ED and has better diagnostic value than CRP.
Keyword
MeSH Terms
Figure
Reference
-
1. Adelberg DE, Bishop MR. Emergencies related to cancer chemotherapy and hematopoietic stem cell transplantation. Emerg Med Clin North Am. 2009; 27:311–331. PMID: 19447314.
Article2. Courtney DM, Aldeen AZ, Gorman SM, Handler JA, Trifilio SM, Parada JP, et al. Cancer-associated neutropenic fever: clinical outcome and economic costs of emergency department care. Oncologist. 2007; 12:1019–1026. PMID: 17766662.
Article3. Rasool Hassan BA, Yusoff ZB, Othman SB. Fever/clinical signs and association with neutropenia in solid cancer patients: bacterial infection as the main cause. Asian Pac J Cancer Prev. 2010; 11:1273–1277. PMID: 21198276.4. Bossink AW, Groeneveld J, Hack CE, Thijs LG. Prediction of mortality in febrile medical patients: How useful are systemic inflammatory response syndrome and sepsis criteria? Chest. 1998; 113:1533–1541. PMID: 9631790.5. Weinstein MP, Towns ML, Quartey SM, Mirrett S, Reimer LG, Parmigiani G, et al. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997; 24:584–602. PMID: 9145732.
Article6. Gendrel D, Raymond J, Coste J, Moulin F, Lorrot M, Guérin S, et al. Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs. viral infections. Pediatr Infect Dis J. 1999; 18:875–881. PMID: 10530583.
Article7. Maruna P, Nedelníková K, Gürlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000; 49(Suppl 1):S57–S61. PMID: 10984072.8. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518. PMID: 8094770.
Article9. Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002; 34:730–751. PMID: 11850858.
Article10. Marshall JC, Reinhart K. International Sepsis Forum. Biomarkers of sepsis. Crit Care Med. 2009; 37:2290–2298. PMID: 19487943.11. Massaro KS, Costa SF, Leone C, Chamone DA. Procalcitonin (PCT) and C-reactive protein (CRP) as severe systemic infection markers in febrile neutropenic adults. BMC Infect Dis. 2007; 7:137. PMID: 18034890.
Article12. Schuttrumpf S, Binder L, Hagemann T, Berkovic D, Trumper L, Binder C. Utility of procalcitonin concentration in the evaluation of patients with malignant diseases and elevated C-reactive protein plasma concentrations. Clin Infect Dis. 2006; 43:468–473. PMID: 16838236.
Article13. Karzai W, Oberhoffer M, Meier-Hellmann A, Reinhart K. Procalcitonin: a new indicator of the systemic response to severe infections. Infection. 1997; 25:329–334. PMID: 9427049.14. Giamarellou H, Giamarellos-Bourboulis EJ, Repoussis P, Galani L, Anagnostopoulos N, Grecka P, et al. Potential use of procalcitonin as a diagnostic criterion in febrile neutropenia: experience from a multicentre study. Clin Microbiol Infect. 2004; 10:628–633. PMID: 15214875.
Article15. Jimeno A, García-Velasco A, del Val O, González-Billalabeitia E, Hernando S, Hernández R, et al. Assessment of procalcitonin as a diagnostic and prognostic marker in patients with solid tumors and febrile neutropenia. Cancer. 2004; 100:2462–2469. PMID: 15160353.
Article16. Hambach L, Eder M, Dammann E, Schrauder A, Sykora KW, Dieterich C, et al. Diagnostic value of procalcitonin serum levels in comparison with C-reactive protein in allogeneic stem cell transplantation. Haematologica. 2002; 87:643–651. PMID: 12031922.17. Bossink AW, Groeneveld AB, Koffeman GI, Becker A. Prediction of shock in febrile medical patients with a clinical infection. Crit Care Med. 2001; 29:25–31. PMID: 11176153.
Article18. Russwurm S, Wiederhold M, Oberhoffer M, Stonans I, Zipfel PF, Reinhart K. Molecular aspects and natural source of procalcitonin. Clin Chem Lab Med. 1999; 37:789–797. PMID: 10536927.
Article19. Hitoglou-Hatzi S, Hatzistilianou M, Gougoustamou D, Rekliti A, Agguridaki CH, Athanassiadou F, et al. Serum adenosine deaminase and procalcitonin concentrations in neutropenic febrile children with acute lymphoblastic leukaemia. Clin Exp Med. 2005; 5:60–65. PMID: 16096855.
Article20. Ruokonen E, Nousiainen T, Pulkki K, Takala J. Procalcitonin concentrations in patients with neutropenic fever. Eur J Clin Microbiol Infect Dis. 1999; 18:283–285. PMID: 10385017.21. Boussekey N, Leroy O, Alfandari S, Devos P, Georges H, Guery B. Procalcitonin kinetics in the prognosis of severe community-acquired pneumonia. Intensive Care Med. 2006; 32:469–472. PMID: 16477418.
Article22. Williams MD, Braun LA, Cooper LM, Johnston J, Weiss RV, Qualy RL, et al. Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit Care. 2004; 8:R291–R298. PMID: 15469571.23. Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R. Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum. 1997; 40:1250–1256. PMID: 9214425.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of Procalcitonin as a Predictive Marker in Accordance with the Severity of Female Patients with Uncomplicated Acute Pyelonephritis
- Prognostic Implications of Procalcitonin and NT-ProBNP in Febrile Neutropenic Patients
- Comparison of the diagnostic performance of initial serum procalcitonin, lactate, and C-reactive protein for predicting bacteremia in female patients with acute pyelonephritis
- Utility of Procalcitonin as an Early Diagnostic Marker of Bacteremia in Patients with Acute Fever
- The Risk Factor of Bacteremia in Children with Febrile Neutropenia due to Chemotherapy