Ann Surg Treat Res.
2015 May;88(5):281-288. 10.4174/astr.2015.88.5.281.
Evaluation of diagnostic biomarkers for acute kidney injury in major burn patients
- Affiliations
-
- 1Department of Surgery and Critical Care, Burn Center, Hallym University Hangang Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. maruchigs@hallym.or.kr
- KMID: 2166997
- DOI: http://doi.org/10.4174/astr.2015.88.5.281
Abstract
- PURPOSE
Acute kidney injury (AKI) in major burn patients is a common complication with high morbidity and mortality. The mainstream treatment is early diagnosis and rapid termination and prevention of the underlying insult. Therefore, it's essential to identify early biomarkers predicting AKI.
METHODS
A total of 85 patients who were admitted to the burn intensive care unit from June 2012 to July 2013 were included in this prospective cohort study. Ten biomarkers (blood urea nitrogen, serum creatinine, urine creatinine, cystatin C, cystatin C glomerular filtration rate, AST, lacate dehydrogenase [LD], creatine kinase, lactic acid, and myoglobin) were obtained at time of admission and evaluated as diagnostic biomarkers to predicting AKI and early AKI.
RESULTS
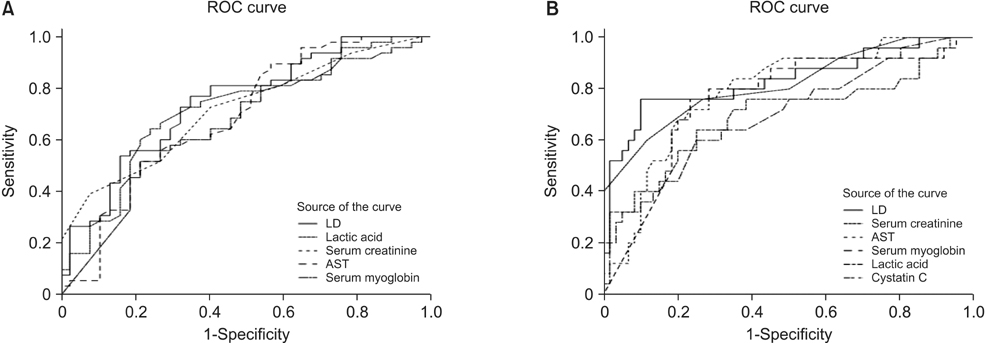
Out of 85 patients, 35 patients were dead and overall mortality was 41.2%. The mean age was 49.4 years and mean percentage of total body surface area was 53.2%. Area under the curve (AUC) of receiver operating characteristic curve of biomarkers on predicting AKI were 0.746, 0.718, and 0.717 in LD, lactic acid, and serum creatinine, respectively. AUC of cystatin C predicting AKI was much lower at 0.555. AUC of biomarkers on predicting early AKI were 0.833, 0.816, 0.790, and 0.759 in LD, serum creatinine, AST, and serum myoglobin.
CONCLUSION
LD, lactic acid and serum creatinine were acceptable as diagnostic biomarkers of AKI and LD, serum creatinine, AST, and serum myoglobin were reasonable as diagnostic biomarkers of early AKI. However, cystatin C was an unfavorable biomarker in major burn patients.
MeSH Terms
-
Acute Kidney Injury*
Area Under Curve
Biomarkers*
Body Surface Area
Burns*
Cohort Studies
Creatine Kinase
Creatinine
Cystatin C
Early Diagnosis
Glomerular Filtration Rate
Humans
Intensive Care Units
L-Lactate Dehydrogenase
Lactic Acid
Mortality
Myoglobin
Nitrogen
Oxidoreductases
Prospective Studies
ROC Curve
Urea
Creatine Kinase
Creatinine
Cystatin C
L-Lactate Dehydrogenase
Lactic Acid
Myoglobin
Nitrogen
Oxidoreductases
Urea
Figure
Reference
-
1. Chung KK, Lundy JB, Matson JR, Renz EM, White CE, King BT, et al. Continuous venovenous hemofiltration in severely burned patients with acute kidney injury: a cohort study. Crit Care. 2009; 13:R62.2. Mustonen KM, Vuola J. Acute renal failure in intensive care burn patients (ARF in burn patients). J Burn Care Res. 2008; 29:227–237.3. Coca SG, Bauling P, Schifftner T, Howard CS, Teitelbaum I, Parikh CR. Contribution of acute kidney injury toward morbidity and mortality in burns: a contemporary analysis. Am J Kidney Dis. 2007; 49:517–523.4. Holm C, Horbrand F, von Donnersmarck GH, Muhlbauer W. Acute renal failure in severely burned patients. Burns. 1999; 25:171–178.5. Ibrahim AE, Sarhane KA, Fagan SP, Goverman J. Renal dysfunction in burns: a review. Ann Burns Fire Disasters. 2013; 26:16–25.6. Belgian Outcome in Burn Injury Study Group. Development and validation of a model for prediction of mortality in patients with acute burn injury. Br J Surg. 2009; 96:111–117.7. Brusselaers N, Juhasz I, Erdei I, Monstrey S, Blot S. Evaluation of mortality following severe burns injury in Hungary: external validation of a prediction model developed on Belgian burn data. Burns. 2009; 35:1009–1014.8. Colpaert K, Hoste EA. Acute kidney injury in burns: a story of volume and inflammation. Crit Care. 2008; 12:192.9. Zager RA, Johnson AC, Becker K. Renal cortical lactate dehydrogenase: a useful, accurate, quantitative marker of in vivo tubular injury and acute renal failure. PLoS One. 2013; 8:e66776.10. Bonventre JV, Vaidya VS, Schmouder R, Feig P, Dieterle F. Next-generation biomarkers for detecting kidney toxicity. Nat Biotechnol. 2010; 28:436–440.11. Coca SG, Yalavarthy R, Concato J, Parikh CR. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008; 73:1008–1016.12. Rodriguez E, Soler MJ, Rap O, Barrios C, Orfila MA, Pascual J. Risk factors for acute kidney injury in severe rhabdomyolysis. PLoS One. 2013; 8:e82992.13. Kosmadakis G, Michail O, Filiopoulos V, Papadopoulou P, Michail S. Acute kidney injury due to rhabdomyolysis in narcotic drug users. Int J Artif Organs. 2011; 34:584–588.14. Jochmans I, Lerut E, van Pelt J, Monbaliu D, Pirenne J. Circulating AST, H-FABP, and NGAL are early and accurate biomarkers of graft injury and dysfunction in a preclinical model of kidney transplantation. Ann Surg. 2011; 254:784–791.15. Westhuyzen J, Endre ZH, Reece G, Reith DM, Saltissi D, Morgan TJ. Measurement of tubular enzymuria facilitates early detection of acute renal impairment in the intensive care unit. Nephrol Dial Transplant. 2003; 18:543–551.16. Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982; 11:260–262.17. Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26:1793–1800.18. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004; 8:R204–R212.19. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982; 143:29–36.20. Brusselaers N, Monstrey S, Colpaert K, Decruyenaere J, Blot SI, Hoste EA. Outcome of acute kidney injury in severe burns: a systematic review and meta-analysis. Intensive Care Med. 2010; 36:915–925.21. Kellum JA, Levin N, Bouman C, Lameire N. Developing a consensus classification system for acute renal failure. Curr Opin Crit Care. 2002; 8:509–514.22. Chrysopoulo MT, Jeschke MG, Dziewulski P, Barrow RE, Herndon DN. Acute renal dysfunction in severely burned adults. J Trauma. 1999; 46:141–144.23. Emara SS, Alzaylai AA. Renal failure in burn patients: a review. Ann Burns Fire Disasters. 2013; 26:12–15.24. Rivers EP, Coba V, Whitmill M. Early goal-directed therapy in severe sepsis and septic shock: a contemporary review of the literature. Curr Opin Anaesthesiol. 2008; 21:128–140.25. Soni SS, Pophale R, Ronco C. New biomarkers for acute renal injury. Clin Chem Lab Med. 2011; 49:1257–1263.26. Jung YJ, Lee HR, Kwon OJ. Comparison of serum cystatin C and creatinine as a marker for early detection of decreasing glomerular filtration rate in renal transplants. J Korean Surg Soc. 2012; 83:69–74.27. Gonzalez F, Vincent F. Biomarkers for acute kidney injury in critically ill patients. Minerva Anestesiol. 2012; 78:1394–1403.28. Odutayo A, Cherney D. Cystatin C and acute changes in glomerular filtration rate. Clin Nephrol. 2012; 78:64–75.29. Cai X, Long Z, Lin L, Feng Y, Zhou N, Mai Q. Serum cystatin C is an early biomarker for assessment of renal function in burn patients. Clin Chem Lab Med. 2012; 50:667–671.