Allergy Asthma Immunol Res.
2014 Jan;6(1):33-38. 10.4168/aair.2014.6.1.33.
Can Fecal Calprotectin Level Be Used as a Markers of Inflammation in the Diagnosis and Follow-Up of Cow's Milk Protein Allergy?
- Affiliations
-
- 1Department of Pediatric Gastroenterology, Hepatology and Nutrition, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, Turkey. bosporus2006@hotmail.com
- 2Department of Pediatrics, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, Turkey.
- 3Department of Pediatric Allergy, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, Turkey.
- KMID: 2166926
- DOI: http://doi.org/10.4168/aair.2014.6.1.33
Abstract
- PURPOSE
Calprotectin is a cytosolic protein with immunomodulatory, antimicrobial, and antiproliferative actions. The concentration of calprotectin increases in infection, inflammation, and malignancy. We determined if calprotectin can be used as a marker for the diagnosis and follow-up of bowel inflammation in cow's milk protein allergy (CMPA).
METHODS
In total, 32 patients newly diagnosed with CMPA were included (24 IgE-mediated, 8 non-IgE-mediated). In all subjects, a complete blood count, total IgE, cow's milk-specific IgE, and fecal calprotectin (FC) were assessed before and after a cow's milk protein (CMP) elimination diet was started. The results were compared with those of 39 healthy children.
RESULTS
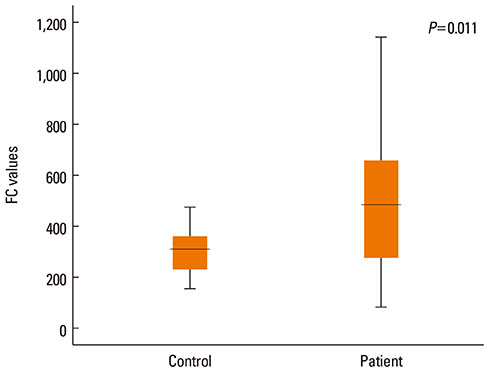
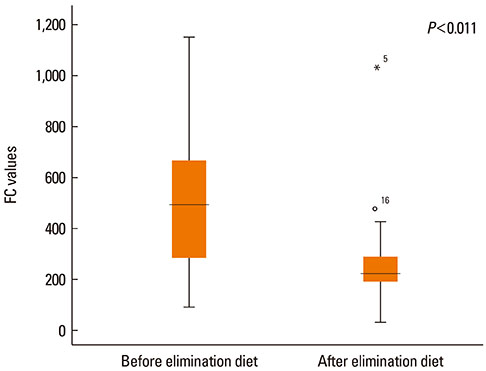
The mean FC value before the CMP elimination diet was 516+/-311 microg/g in the 32 patients with CMPA and 296+/-94 microg/g in the control group (P=0.011). The mean FC value after the diet in these patients was 254+/-169 microg/g, which was significantly different from the mean value before the CMP elimination diet (P<0.001). When we compared FC levels before the CMP elimination diet in the IgE-mediated group with the control group, we found no significant statistical difference (P=0.142). The mean FC value before the CMP elimination diet was 886+/-278 microg/g in the non-IgE-mediated group and 296+/-94 microg/g in the control group; this difference was statistically significant (P<0.001). In the IgE-mediated and non-IgE-mediated groups, FC values after CMP elimination diet were 218+/-90 microg/g and 359+/-288 microg/g, respectively, and FC values before CMP elimination diet were 392+/-209 microg/g and 886+/-278 microg/g, respectively; these differences were statistically significant (P=0.001 and P=0.025, respectively).
CONCLUSIONS
FC levels may be a useful marker for follow-up treatment and recurrence determination in CMPA.
MeSH Terms
Figure
Reference
-
1. Arvola T, Ruuska T, Keränen J, Hyöty H, Salminen S, Isolauri E. Rectal bleeding in infancy: clinical, allergological, and microbiological examination. Pediatrics. 2006; 117:e760–e768.2. Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S. Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis. J Korean Med Sci. 2007; 22:213–217.3. Eigenmann PA. Mechanisms of food allergy. Pediatr Allergy Immunol. 2009; 20:5–11.4. Chehade M. IgE and non-IgE-mediated food allergy: treatment in 2007. Curr Opin Allergy Clin Immunol. 2007; 7:264–268.5. Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004; 113:805–819.6. NIAID-Sponsored Expert Panel. Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ, Arshad SH, Bahna SL, Beck LA, Byrd-Bredbenner C, Camargo CA Jr, Eichenfield L, Furuta GT, Hanifin JM, Jones C, Kraft M, Levy BD, Lieberman P, Luccioli S, McCall KM, Schneider LC, Simon RA, Simons FE, Teach SJ, Yawn BP, Schwaninger JM. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010; 126:S1–S58.7. Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, Mearin ML, Papadopoulou A, Ruemmele FM, Staiano A, Schäppi MG, Vandenplas Y. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012; 55:221–229.8. Klemola T, Vanto T, Juntunen-Backman K, Kalimo K, Korpela R, Varjonen E. Allergy to soy formula and to extensively hydrolyzed whey formula in infants with cow's milk allergy: a prospective, randomized study with a follow-up to the age of 2 years. J Pediatr. 2002; 140:219–224.9. Eggesbø M, Botten G, Halvorsen R, Magnus P. The prevalence of CMA/CMPI in young children: the validity of parentally perceived reactions in a population-based study. Allergy. 2001; 56:393–402.10. Berntzen HB, Olmez U, Fagerhol MK, Munthe E. The leukocyte protein L1 in plasma and synovial fluid from patients with rheumatoid arthritis and osteoarthritis. Scand J Rheumatol. 1991; 20:74–82.11. Dunlop O, Bruun JN, Myrvang B, Fagerhol MK. Calprotectin in cerebrospinal fluid of the HIV infected: a diagnostic marker of opportunistic central nervous system infection? Scand J Infect Dis. 1991; 23:687–689.12. Cuida M, Brun JG, Tynning T, Jonsson R. Calprotectin levels in oral fluids: the importance of collection site. Eur J Oral Sci. 1995; 103:8–10.13. Holt J, Fagerhol MK, Dale I. Quantitation of a leukocyte protein (L1) in urine. Acta Paediatr Scand. 1983; 72:615–616.14. Isaksen B, Fagerhol MK. Calprotectin inhibits matrix metalloproteinases by sequestration of zinc. Mol Pathol. 2001; 54:289–292.15. Canani RB, de Horatio LT, Terrin G, Romano MT, Miele E, Staiano A, Rapacciuolo L, Polito G, Bisesti V, Manguso F, Vallone G, Sodano A, Troncone R. Combined use of noninvasive tests is useful in the initial diagnostic approach to a child with suspected inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2006; 42:9–15.16. Berni Canani R, Rapacciuolo L, Romano MT, Tanturri de Horatio L, Terrin G, Manguso F, Cirillo P, Paparo F, Troncone R. Diagnostic value of faecal calprotectin in paediatric gastroenterology clinical practice. Dig Liver Dis. 2004; 36:467–470.17. von Roon AC, Karamountzos L, Purkayastha S, Reese GE, Darzi AW, Teare JP, Paraskeva P, Tekkis PP. Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am J Gastroenterol. 2007; 102:803–813.18. Røseth AG, Schmidt PN, Fagerhol MK. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scand J Gastroenterol. 1999; 34:50–54.19. Fagerberg UL, Lööf L, Merzoug RD, Hansson LO, Finkel Y. Fecal calprotectin levels in healthy children studied with an improved assay. J Pediatr Gastroenterol Nutr. 2003; 37:468–472.20. Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker of intestinal inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:524–534.21. Nielsen RG, Fenger C, Bindslev-Jensen C, Husby S. Eosinophilia in the upper gastrointestinal tract is not a characteristic feature in cow's milk sensitive gastro-oesophageal reflux disease. Measurement by two methodologies. J Clin Pathol. 2006; 59:89–94.22. Ezri J, Nydegger A. Pediatrics. Fecal calprotectin in children: use and interpretation. Rev Med Suisse. 2011; 7:69–70.23. Olafsdottir E, Aksnes L, Fluge G, Berstad A. Faecal calprotectin levels in infants with infantile colic, healthy infants, children with inflammatory bowel disease, children with recurrent abdominal pain and healthy children. Acta Paediatr. 2002; 91:45–50.24. Baldassarre ME, Laforgia N, Fanelli M, Laneve A, Grosso R, Lifschitz C. Lactobacillus GG improves recovery in infants with blood in the stools and presumptive allergic colitis compared with extensively hydrolyzed formula alone. J Pediatr. 2010; 156:397–401.