Allergy Asthma Immunol Res.
2016 Jan;8(1):22-31. 10.4168/aair.2016.8.1.22.
Prevalence, Severity, and Treatment of Recurrent Wheezing During the First Year of Life: A Cross-Sectional Study of 12,405 Latin American Infants
- Affiliations
-
- 1Department of Pediatric Respiratory Medicine, Hospital El Pino, University of Santiago de Chile (USACH), Santiago, Chile. jmallol@vtr.net
- 2Division of Allergy, Clinical Immunology and Rheumatology, Department of Pediatrics, Federal University of Sao Paulo (UNIFESP), Sao Paulo, Brazil.
- 3Pediatric Respiratory and Allergy Units, "Virgen de la Arrixaca" University Children's Hospital, University of Murcia, and IMIB Research Institute, Murcia, Spain.
- 4Department of Pediatrics, Hospital de Clinicas, Federal University of Parana (UFPR), Curitiba, Brazil.
- 5Pediatric Asthma Prevention Program (PIPA), Uruguaiana, Brazil.
- 6Hospital de Ninos "Ricardo Gutierrez", Buenos Aires, Argentina.
- 7Escuela de Medicina, Universidad Industrial de Santander, Bucaramanga, Colombia.
- 8Section of Allergy and Clinical Immunology, British American Hospital, Lima, Peru.
- 9Hospital de Base de Sao Jose do Rio Preto, Faculty of Medicine of Sao Jose do Rio Preto, Sao Paulo, Brazil.
- 10Department of Pediatrics, Federal University of Mato Grosso, Cuiaba, Brazil.
- 11Clinica Pediatrica "B". Hospital Pereira Rossell, Facultad Medicina, Universidad de la Republica, Montevideo, Uruguay.
- KMID: 2166646
- DOI: http://doi.org/10.4168/aair.2016.8.1.22
Abstract
- PURPOSE
This study aimed to determine the prevalence and severity of recurrent wheezing (RW) defined as > or =3 episodes of wheezing, risk factors, and treatments prescribed during the first year of life in Latin American infants.
METHODS
In this international, cross-sectional, and community-based study, parents of 12,405 infants from 11 centers in 6 South American countries (Argentina, Brazil, Chile, Colombia, Peru, and Uruguay) completed a questionnaire about wheezing and associated risk/protective factors, asthma medications, and the frequency of and indications for the prescription of antibiotics and paracetamol during the first year of life.
RESULTS
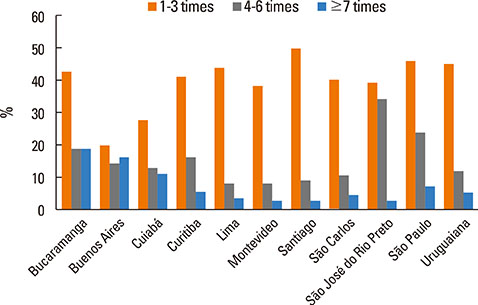
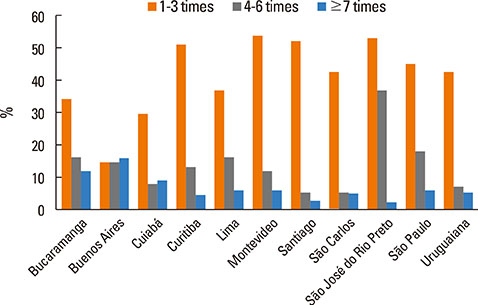
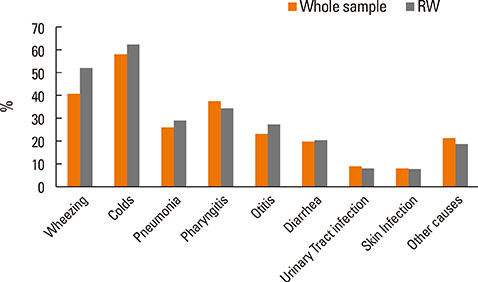
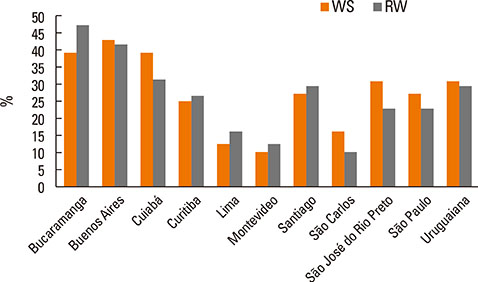
The prevalence of RW was 16.6% (95% CI 16.0-17.3); of the 12,405 infants, 72.7% (95% CI 70.7-74.6) visited the Emergency Department for wheezing, and 29.7% (27.7-31.7) was admitted. Regarding treatment, 49.1% of RW infants received inhaled corticosteroids, 55.7% oral corticosteroids, 26.3% antileukotrienes, 22.9% antibiotics > or =4 times mainly for common colds, wheezing, and pharyngitis, and 57.5% paracetamol > or =4 times. Tobacco smoking during pregnancy, household income per month <1,000 USD, history of parental asthma, male gender, and nursery school attendance were significant risk factors for higher prevalence and severity of RW, whereas breast-feeding for at least 3 months was a significant protective factor. Pneumonia and admissions for pneumonia were significantly higher in infants with RW as compared to the whole sample (3.5-fold and 3.7-fold, respectively).
CONCLUSIONS
RW affects 1.6 out of 10 infants during the first year of life, with a high prevalence of severe episodes, frequent visits to the Emergency Department, and frequent admissions for wheezing. Besides the elevated prescription of asthma medications, there is an excessive use of antibiotics and paracetamol in infants with RW and also in the whole sample, which is mainly related to common colds.
MeSH Terms
-
Acetaminophen
Adrenal Cortex Hormones
Anti-Bacterial Agents
Asthma
Brazil
Chile
Colombia
Common Cold
Cross-Sectional Studies*
Emergency Service, Hospital
Epidemiology
Family Characteristics
Humans
Infant*
Male
Parents
Peru
Pharyngitis
Pneumonia
Pregnancy
Prescriptions
Prevalence*
Respiratory Sounds*
Risk Factors
Schools, Nursery
Smoking
Acetaminophen
Adrenal Cortex Hormones
Anti-Bacterial Agents
Figure
Reference
-
1. Kuehni CE, Strippoli MP, Low N, Brooke AM, Silverman M. Wheeze and asthma prevalence and related health-service use in white and south Asian pre-schoolchildren in the United Kingdom. Clin Exp Allergy. 2007; 37:1738–1746.2. Cavalcanti Dela Bianca AC, Wandalsen G, Prestes E, Lamenha M, Bessa O, Chong Neto H, et al. Treatment of wheezing in Brazilian infants in the first year of life. Pediatr Allergy Immunol. 2014; 25:201–203.3. Mallol J, García-Marcos L, Solé D, Brand P. EISL Study Group. International prevalence of recurrent wheezing during the first year of life: variability, treatment patterns and use of health resources. Thorax. 2010; 65:1004–1009.4. Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011; 128:1053–1061.5. Mangione-Smith R, Krogstad P. Antibiotic prescription with asthma medications: why is it so common? Pediatrics. 2011; 127:1174–1176.6. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998; 279:875–877.7. Beasley R, Clayton T, Crane J, von Mutius E, Lai CK, Montefort S, et al. Association between paracetamol use in infancy and childhood, and risk of asthma, rhinoconjunctivitis, and eczema in children aged 6-7 years: analysis from Phase Three of the ISAAC programme. Lancet. 2008; 372:1039–1048.8. Foliaki S, Pearce N, Björkstén B, Mallol J, Montefort S, von Mutius E, et al. Antibiotic use in infancy and symptoms of asthma, rhinoconjunctivitis, and eczema in children 6 and 7 years old: International Study of Asthma and Allergies in Childhood Phase III. J Allergy Clin Immunol. 2009; 124:982–989.9. Heintze K, Petersen KU. The case of drug causation of childhood asthma: ATB and PCM. Eur J Clin Pharmacol. 2013; 69:1197–1209.10. Penders J, Kummeling I, Thijs C. Infant antibiotic use and wheeze and asthma risk: a systematic review and meta-analysis. Eur Respir J. 2011; 38:295–302.11. Almqvist C, Wettermark B, Hedlin G, Ye W, Lundholm C. Antibiotics and asthma medication in a large register-based cohort study - confounding, cause and effect. Clin Exp Allergy. 2012; 42:104–111.12. Lapin B, Piorkowski J, Ownby D, Wagner-Cassanova C, Freels S, Chavez N, et al. The relationship of early-life antibiotic use with asthma in at-risk children. J Allergy Clin Immunol. 2014; 134:728–729.13. Schnabel E, Heinrich J. LISA Study Group. Respiratory tract infections and not paracetamol medication during infancy are associated with asthma development in childhood. J Allergy Clin Immunol. 2010; 126:1071–1073.14. Shaheen SO, Newson RB, Henderson AJ, Headley JE, Stratton FD, Jones RW, et al. Prenatal paracetamol exposure and risk of asthma and elevated immunoglobulin E in childhood. Clin Exp Allergy. 2005; 35:18–25.15. Gonzalez-Barcala FJ, Pertega S, Perez Castro T, Sampedro M, Sanchez Lastres J J, San Jose Gonzalez MA, et al. Exposure to paracetamol and asthma symptoms. Eur J Public Health. 2013; 23:706–710.16. Lowe AJ, Carlin JB, Bennett CM, Hosking CS, Allen KJ, Robertson CF, et al. Paracetamol use in early life and asthma: prospective birth cohort study. BMJ. 2010; 341:c4616.17. Rebordosa C, Kogevinas M, Sørensen HT, Olsen J. Pre-natal exposure to paracetamol and risk of wheezing and asthma in children: a birth cohort study. Int J Epidemiol. 2008; 37:583–590.18. Amberbir A, Medhin G, Hanlon C, Britton J, Davey G, Venn A. Effects of early life paracetamol use on the incidence of allergic disease and sensitization: 5 year follow-up of an Ethiopian birth cohort. PLoS One. 2014; 9:e93869.19. Garcia-Marcos L, Mallol J, Solé D, Brand PL. EISL Study Group. International study of wheezing in infants: risk factors in affluent and non-affluent countries during the first year of life. Pediatr Allergy Immunol. 2010; 21:878–888.20. Bianca AC, Wandalsen GF, Miyagi K, Camargo L, Cezarin D, Mallol J, et al. International Study of Wheezing in Infants (EISL): validation of written questionnaire for children aged below 3 years. J Investig Allergol Clin Immunol. 2009; 19:35–42.21. Chong Neto HJ, Rosario N, Dela Bianca AC, Solé D, Mallol J. Validation of a questionnaire for epidemiologic studies of wheezing in infants. Pediatr Allergy Immunol. 2007; 18:86–87.22. Mallol J, García-Marcos L, Aguirre V, Martinez-Torres A, Perez-Fernández V, Gallardo A, et al. The International Study of Wheezing in Infants: questionnaire validation. Int Arch Allergy Immunol. 2007; 144:44–50.23. Murray JS, Amin PM. Overprescribing antibiotics in children: an enduring public health concern. J Spec Pediatr Nurs. 2014; 19:266–269.24. Cadieux G, Tamblyn R, Dauphinee D, Libman M. Predictors of inappropriate antibiotic prescribing among primary care physicians. CMAJ. 2007; 177:877–883.25. Eckel N, Sarganas G, Wolf IK, Knopf H. Pharmacoepidemiology of common colds and upper respiratory tract infections in children and adolescents in Germany. BMC Pharmacol Toxicol. 2014; 15:44.26. Harnden A, Perera R, Brueggemann AB, Mayon-White R, Crook DW, Thomson A, et al. Respiratory infections for which general practitioners consider prescribing an antibiotic: a prospective study. Arch Dis Child. 2007; 92:594–597.27. Martinez FD. The connection between early life wheezing and subsequent asthma: the viral march. Allergol Immunopathol (Madr). 2009; 37:249–251.28. Saglani S. Viral infections and the development of asthma in children. Ther Adv Infect Dis. 2013; 1:139–150.29. Beigelman A, King TS, Mauger D, Zeiger RS, Strunk RC, Kelly HW, et al. Do oral corticosteroids reduce the severity of acute lower respiratory tract illnesses in preschool children with recurrent wheezing? J Allergy Clin Immunol. 2013; 131:1518–1525.30. Pelkonen AS, Malmström K, Sarna S, Kajosaari M, Klemola T, Malmberg LP, et al. The effect of montelukast on respiratory symptoms and lung function in wheezy infants. Eur Respir J. 2013; 41:664–670.31. Bueso A, Figueroa M, Cousin L, Hoyos W, Martínez-Torres AE, Mallol J, et al. Poverty-associated risk factors for wheezing in the first year of life in Honduras and El Salvador. Allergol Immunopathol (Madr). 2010; 38:203–212.32. Mallol J, Andrade R, Auger F, Rodríguez J, Alvarado R, Figueroa L. Wheezing during the first year of life in infants from low-income population: a descriptive study. Allergol Immunopathol (Madr). 2005; 33:257–263.33. Margolis PA, Greenberg RA, Keyes LL, LaVange LM, Chapman RS, Denny FW, et al. Lower respiratory illness in infants and low socioeconomic status. Am J Public Health. 1992; 82:1119–1126.34. Klinnert MD, Price MR, Liu AH, Robinson JL. Morbidity patterns among low-income wheezing infants. Pediatrics. 2003; 112:49–57.35. Progress and inequity in Latin America. Lancet. 2007; 370:1589.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of gastroesophageal reflux in infants with recurrent wheezing
- A study of total eosinophil count, total IgE concentration and sensitization of house dust mite allergens as atopic parameters in recurrent wheezing infants
- The Relationship between the Time of First Respiratory Syncytial Virus Bronchiolitis and Later Wheezing and Asthma Development
- Bronchial Asthma after Early Infant Bronchiolitis: A Follow-up Until 5 Years of Age
- Relationship between Silent Gastroesophageal Reflux and Food Sensitization in Infants and Young Children with Recurrent Wheezing