Considerable Variability of Procedural Sedation and Analgesia Practices for Gastrointestinal Endoscopic Procedures in Europe
- Affiliations
-
- 1Division of Anaesthesiology, Intensive Care and Emergency Medicine, University Medical Centre Utrecht, Utrecht, Netherlands. H.H.B.Vaessen@umcutrecht.nl
- KMID: 2166549
- DOI: http://doi.org/10.5946/ce.2016.49.1.47
Abstract
- BACKGROUND/AIMS
The use of moderate to deep sedation for gastrointestinal endoscopic procedures has increased in Europe considerably. Because this level of sedation is a risky medical procedure, a number of international guidelines have been developed. This survey aims to review if, and if so which, quality aspects have been included in new sedation practices when compared to traditional uncontrolled sedation practices.
METHODS
A questionnaire was sent to the National Associations of Nurse Anesthetists in Europe and the National Delegates of the European Section and Board of Anaesthesiology from January 2012 to August 2012.
RESULTS
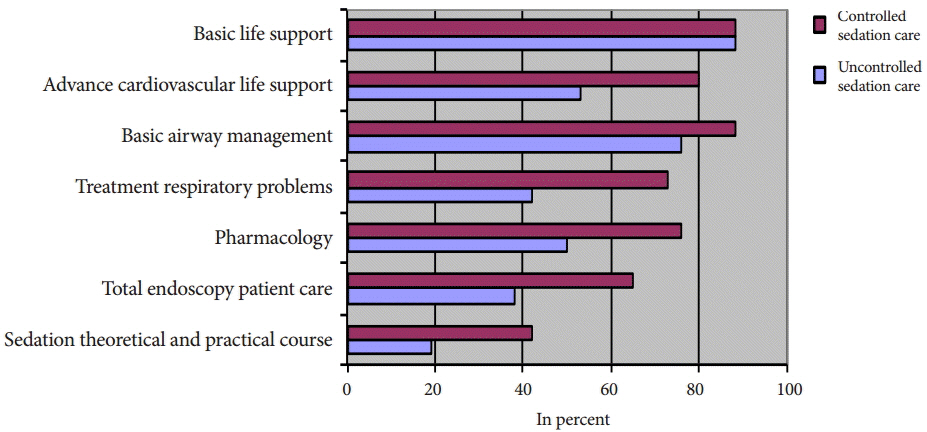
Huge variation in practices for moderate to deep sedation were identified between and within European countries in terms of safety, type of practitioners, responsibilities, monitoring, informed consent, patient satisfaction, complication registration, and training requirements. Seventy-five percent of respondents were not familiar with international sedation guidelines. Safe sedation practices (mainly propofol-based moderate to deep sedation) are rapidly gaining popularity.
CONCLUSIONS
The risky medical procedure of moderate to deep sedation has become common practice for gastrointestinal endoscopy. Safe sedation practices requiring adequate selection of patients, adequate monitoring, training of sedation practitioners, and adequate after-care, are gaining attention in a field that is in transition from uncontrolled sedation care to controlled sedation care.
MeSH Terms
Figure
Cited by 3 articles
-
Safety and Recipient Satisfaction of Propofol Sedation in Outpatient Endoscopy: A 24-Hour Prospective Investigation Using a Questionnaire Survey
Yoshihide Kanno, Tetsuya Ohira, Yoshihiro Harada, Shinsuke Koshita, Takahisa Ogawa, Hiroaki Kusunose, Yoshiki Koike, Taku Yamagata, Toshitaka Sakai, Kaori Masu, Keisuke Yonamine, Kazuaki Miyamoto, Megumi Tanaka, Tomohiro Shimada, Fumisato Kozakai, Kazuki Endo, Haruka Okano, Daichi Komabayashi, Takeshi Shimizu, Shohei Suzuki, Kei Ito
Clin Endosc. 2021;54(3):340-347. doi: 10.5946/ce.2020.138.Risk Factors for Prolonged Hospital Stay after Endoscopy
Toshihiro Nishizawa, Shuntaro Yoshida, Osamu Toyoshima, Tatsuya Matsuno, Masataka Irokawa, Toru Arano, Hirotoshi Ebinuma, Hidekazu Suzuki, Takanori Kanai, Kazuhiko Koike
Clin Endosc. 2021;54(6):851-856. doi: 10.5946/ce.2020.292.Sedation for Gastrointestinal Endoscopy: Practical Issues in Patient Safety and Quality Management
Seung Bae Yoon, Young-Seok Cho
Clin Endosc. 2016;49(1):1-3. doi: 10.5946/ce.2016.49.1.1.
Reference
-
1. Hirschowitz BI, Curtiss LE, Peters CW, Pollard HM. Demonstration of a new gastroscope, the fiberscope. Gastroenterology. 1958; 35:50.
Article2. Hirschowitz BI. Endoscopy: 40 years since fiber optics. Any light at the end of the tunnel? Dig Surg. 2000; 17:115–117.3. Garborg KK, Løberg M, Matre J, et al. Reduced pain during screening colonoscopy with an ultrathin colonoscope: a randomized controlled trial. Endoscopy. 2012; 44:740–746.
Article4. Dumonceau JM, Riphaus A, Aparicio JR, et al. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: non-anaesthesiologist administration of propofol for GI endoscopy. Eur J Anaesthesiol. 2010; 27:1016–1030.
Article5. Dumonceau JM, Riphaus A, Aparicio JR, et al. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: non-anesthesiologist administration of propofol for GI endoscopy. Endoscopy. 2010; 42:960–974.
Article6. American Society of Anesthesiologists. Distinguishing monitored anesthesia care (“MAC”) from moderate sedation/analgesia (conscious sedation) [Internet]. Parkridge: American Society of Anesthesiologists;c1995. [cited 2015 Dec 30]. Available from: file:///C:/Users/USER/Downloads/distinguishing-monitored-anesthesia-care-from-moderate-sedation-analgesia%20(1).pdf.7. Joint Commission Resources Organizations. New definitions, revised standards address the continuum of sedation and anesthesia. Jt Comm Perspect. 2000; 20:10.8. Kweon TD. Sedation under JCI standard. Korean J Anesthesiol. 2011; 61:190–194.
Article9. Eberl S, Polderman JA, Preckel B, Kalkman CJ, Fockens P, Hollmann MW. Is “really conscious” sedation with solely an opioid an alternative to every day used sedation regimes for colonoscopies in a teaching hospital? Midazolam/fentanyl, propofol/alfentanil, or alfentanil only for colonoscopy: a randomized trial. Tech Coloproctol. 2014; 18:745–752.
Article10. American Society of Anesthesiologists. Continuum of depth of sedation: definition of general anaesthesia and levels of sedation/analgesia [Internet]. Parkridge: American Society of Anesthesiologists;c1995. [cited 2015 Dec 30]. Available from: http://bit.ly/11iGIax.11. Waring JP, Baron TH, Hirota WK, et al. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003; 58:317–322.
Article12. Meeusen V, van Zundert A, Hoekman J, Kumar C, Rawal N, Knape H. Composition of the anaesthesia team: a European survey. Eur J Anaesthesiol. 2010; 27:773–779.
Article13. EBA UEMS. The European Section and Board of Anesthesiology is the Anesthesiology branch of UEMS (European Union Medical Specialities) dealing primarily with Anesthesia and Resuscitation, as well as Intensive Care, Emergency and Pain Medicine [Internet]. Brussels: EBA UEMS;c2015. [cited 2015 Dec 30]. Available from: http://www.eba-uems.eu.14. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002; 96:1004–1017.15. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008; 67:910–923.
Article16. Nayar DS, Guthrie WG, Goodman A, et al. Comparison of propofol deep sedation versus moderate sedation during endosonography. Dig Dis Sci. 2010; 55:2537–2544.
Article17. Zippi M, Traversa G, De Felici I, et al. Sedation with propofol in endoscopic retrograde cholangiopancreatography: personal experience. Clin Ter. 2008; 159:19–22.18. Patel S, Vargo JJ, Khandwala F, et al. Deep sedation occurs frequently during elective endoscopy with meperidine and midazolam. Am J Gastroenterol. 2005; 100:2689–2695.
Article19. Schilling D, Rosenbaum A, Schweizer S, Richter H, Rumstadt B. Sedation with propofol for interventional endoscopy by trained nurses in high-risk octogenarians: a prospective, randomized, controlled study. Endoscopy. 2009; 41:295–298.
Article20. Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009; 137:1229–1237.
Article21. Müller M, Wehrmann T, Eckardt AJ. Prospective evaluation of the routine use of a nasopharyngeal airway (Wendl Tube) during endoscopic propofol-based sedation. Digestion. 2014; 89:247–252.
Article22. Perel A. Non-anaesthesiologists should not be allowed to administer propofol for procedural sedation: a Consensus Statement of 21 European National Societies of Anaesthesia. Eur J Anaesthesiol. 2011; 28:580–584.23. Külling D, Orlandi M, Inauen W. Propofol sedation during endoscopic procedures: how much staff and monitoring are necessary? Gastrointest Endosc. 2007; 66:443–449.
Article24. Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002; 97:1159–1163.
Article25. Werner C, Smith A, Van Aken H. Guidelines on non-anaesthesiologist administration of propofol for gastrointestinal endoscopy: a double-edged sword. Eur J Anaesthesiol. 2011; 28:553–555.26. Axon AE. The use of propofol by gastroenterologists: medico-legal issues. Digestion. 2010; 82:110–112.
Article27. von Delius S, Hollweck R, Schmid RM, Frimberger E. Midazolam-pain, but one cannot remember it: a survey among Southern German endoscopists. Eur J Gastroenterol Hepatol. 2007; 19:465–470.
Article28. van Gelder RE, Birnie E, Florie J, et al. CT colonography and colonoscopy: assessment of patient preference in a 5-week follow-up study. Radiology. 2004; 233:328–337.
Article29. Garewal D, Vele L, Waikar P. Anaesthetic considerations for endoscopic retrograde cholangio-pancreatography procedures. Curr Opin Anaesthesiol. 2013; 26:475–480.
Article30. Staff DM, Saeian K, Rochling F, et al. Does open access endoscopy close the door to an adequately informed patient? Gastrointest Endosc. 2000; 52:212–217.
Article31. Ladas SD, Aabakken L, Rey JF, et al. Use of sedation for routine diagnostic upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy Survey of National Endoscopy Society Members. Digestion. 2006; 74:69–77.
Article32. Travis AC, Pievsky D, Saltzman JR. Endoscopy in the elderly. Am J Gastroenterol. 2012; 107:1495–1501.
Article33. Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007; 66:27–34.
Article34. Standards of Practice Committee, Lichtenstein DR, Jagannath S, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008; 68:205–216.
Article35. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.
Article36. Conigliaro R, Rossi A; Italian Society of Digestive Endoscopy (SIED) Sedation Commission. Implementation of sedation guidelines in clinical practice in Italy: results of a prospective longitudinal multicenter study. Endoscopy. 2006; 38:1137–1143.
Article37. Morton NS. Safe sedation? Anaesthesia. 2011; 66:653–655.
Article