Cancer Res Treat.
2006 Jun;38(3):184-188.
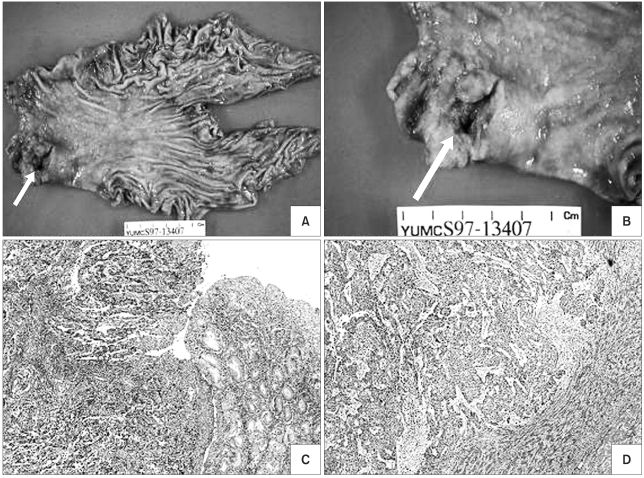
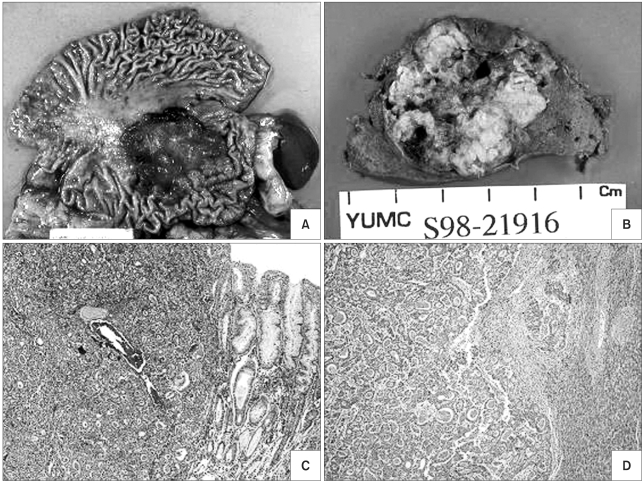
Long-term Survival after Surgical Resection for Liver Metastasis from Gastric Cancer: Two Case Reports
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Cancer Metastasis Research Center, Yonsei University College of Medicine, Seoul, Korea.
- 5Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea. jeunghc1123@yumc.yonsei.ac.kr
Abstract
- Surgical resection of colorectal cancer metastasis to the liver results in a 5-year survival rate of around 40%. Liver metastasis from other cancers such as neuroendocrine carcinoma and genitourinary tumors are also treated effectively with combined liver resection. However, hepatic metastasectomy for liver tumor from gastric cancer hasn't been considered as a standard treatment, and the benefit for this treatment has not been established. We report here on two cases of gastrectomy and combined liver resection for synchronous liver metastasis without any evidence of other metastatic lesions, and these two patients have survived for more than 7 years without evidence of disease recurrence. In conclusion, for patients with hepatic metastasis from gastric cancer, combined surgical resection of the liver metastasis should be considered as a treatment option when metastasis to other sites can be excluded.
MeSH Terms
Figure
Reference
-
1. Ochiai T, Sasako M, Mizuno S, Kinoshita T, Takayama T, Kosuge T, et al. Hepatic resection for metastatic tumours from gastric cancer: analysis of prognostic factors. Br J Surg. 1994; 81:1175–1178. PMID: 7953354.
Article2. Yoshikawa K, Kitaoka H. Clinicopathologic studies of gastric cancer with metastasis to the liver: based on the case detected at initial surgery. Jpn Clin Oncol. 1984; 14:81–86.3. Okuyama K, Isono K, Juan IK, Onoda S, Ochiai T, Yamamoto Y, et al. Evaluation of treatment for gastric cancer with liver metastasis. Cancer. 1985; 55:2498–2505. PMID: 3986746.
Article4. Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995; 19:59–71. PMID: 7740812.
Article5. Taylor M, Forster J, Langer B, Taylor BR, Greig PD, Mahut C. A study of prognostic factors for hepatic resection for colorectal metastases. Am J Surg. 1997; 173:467–471. PMID: 9207156.
Article6. Yamamoto J, Shimada K, Kosuge T, Yamasaki S, Sakamoto M, Fukuda H. Factors influencing survival of patients undergoing hepatectomy for colorectal metastases. Br J Surg. 1999; 86:332–337. PMID: 10201774.
Article7. Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, Kosuge T, et al. Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg. 2000; 231:487–499. PMID: 10749608.8. Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, et al. Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. Am J Surg. 2001; 181:153–159. PMID: 11425058.
Article9. Gayowski TJ, Iwatsuki S, Madariaga JR, Selby R, Todo S, Irish W, et al. Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery. 1994; 116:703–710. PMID: 7940169.10. Miyazaki M, Itoh H, Nakagawa K, Ambiru S, Shimizu H, Togawa A, et al. Hepatic resection of liver metastases from gastric carcinoma. Am J Gastroenterol. 1997; 92:490–493. PMID: 9068476.11. Okano K, Maeba T, Ishimura K, Karasawa Y, Goda F, Wakabayashi H, et al. Hepatic resection for metastatic tumors from gastric cancer. Ann Surg. 2002; 235:86–91. PMID: 11753046.
Article12. Imamura H, Matsuyama Y, Shimada R, Kubota M, Nakayama A, Kobayashi A, et al. A study of factors influencing prognosis after resection of hepatic metastases from colorectal and gastric carcinoma. Am J Gastroenterol. 2001; 96:3178–3184. PMID: 11721768.
Article13. Ambiru S, Miyazaki M, Ito H, Nakagawa K, Shimizu H, Yoshidome H, et al. Benefit and limits of hepatic resection for gastric metastasis. Am J Surg. 2001; 181:279–283. PMID: 11376587.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic Resection in Patients with Liver Metastasis from Gastric Cancer
- Hepatic Solitary Metastasis of Gastric Cancer: Radiofrequency
- Long Term Survival in Patient with Hepatocellular Carcinoma after Surgical Resection of Brain Metastasis: A Case Report
- A Case of Long Term Survival in Patient with Early Intrahepatic Recurrence and Extrahepatic Metastasis after Curative Resection of Hepatocellular Carcinoma
- Long-term Outcome after Endoscopic Resection for Early Gastric Cancer in Korea