Ann Rehabil Med.
2015 Jun;39(3):366-373. 10.5535/arm.2015.39.3.366.
Efficacy of Systemic Postoperative Pulmonary Rehabilitation After Lung Resection Surgery
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pusan National University School of Medicine, Busan, Korea. yi0314@gmail.com
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Department of Rehabilitation Medicine, Medwill Hospital, Busan, Korea.
- 4Regional Center for Respiratory Diseases, Pusan National University Hospital, Busan, Korea.
- 5Department of Thoracic and Cardiovascular Surgery, Pusan National University School of Medicine, Busan, Korea.
- 6Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea.
- 7Department of Biostatistics, Clinical Trial Center, Pusan National University Hospital, Busan, Korea.
- KMID: 2165639
- DOI: http://doi.org/10.5535/arm.2015.39.3.366
Abstract
OBJECTIVE
To investigate the efficacy of systemic pulmonary rehabilitation (PR) after lung resection in patients with lung cancer.
METHODS
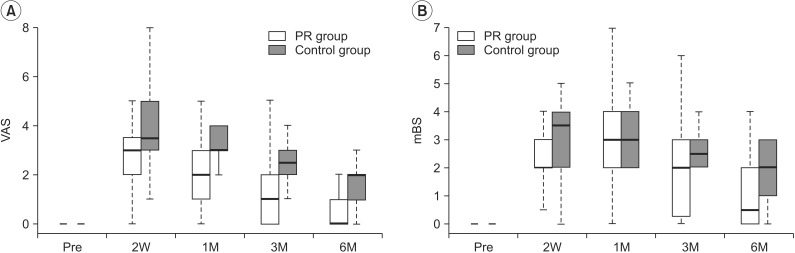
Forty-one patients undergoing lung resection were enrolled and classified into the experimental (n=31) and control groups (n=10). The experimental group underwent post-operative systemic PR which was conducted 30 min/day on every hospitalization day by an expert physical therapist. The control group received the same education about the PR exercises and were encouraged to self-exercise without supervision of the physical therapist. The PR group was taught a self-PR program and feedback was provided regularly until 6 months after surgery. We conducted pulmonary function testing (PFT) and used a visual analog scale (VAS) to evaluate pain, and the modified Borg Dyspnea Scale (mBS) to measure perceived respiratory exertion shortly before and 2 weeks, 1, 3, and 6 months after surgery.
RESULTS
A significant improvement on the VAS was observed in patients who received systemic PR >3 months. Significant improvements in forced vital capacity (FVC) and mBS score were observed in patients who received systemic PR >6 months (p<0.05). Other PFT results were not different compared with those in the control group.
CONCLUSION
Patients who received lung resection suffered a significant decline in functional reserve and increases in pain and subjective dyspnea deteriorating quality of life (QoL). Systemic PR supervised by a therapist helped improve reduced pulmonary FVC and QoL and minimized discomfort during the postoperative periods in patients who underwent lung resection.
MeSH Terms
Figure
Cited by 1 articles
-
Recent Trends in Rehabilitation for Cancer Patients
Kwan-Sik Seo
Ann Rehabil Med. 2022;46(3):111-113. doi: 10.5535/arm.22072.
Reference
-
1. Derom E, Marchand E, Troosters T. Pulmonary rehabilitation in chronic obstructive pulmonary disease. Ann Readapt Med Phys. 2007; 50:615–626. PMID: 17559963.2. Bobbio A, Chetta A, Ampollini L, Primomo GL, Internullo E, Carbognani P, et al. Preoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancer. Eur J Cardiothorac Surg. 2008; 33:95–98. PMID: 18006327.
Article3. Chetta A, Castagnaro A, Foresi A, Del Donno M, Pisi G, Malorgio R, et al. Assessment of breathlessness perception by Borg scale in asthmatic patients: reproducibility and applicability to different stimuli. J Asthma. 2003; 40:323–329. PMID: 12807177.
Article4. Rochester CL. Pulmonary rehabilitation for patients who undergo lung-volume-reduction surgery or lung transplantation. Respir Care. 2008; 53:1196–1202. PMID: 18718039.5. Pearson FG. Current status of surgical resection for lung cancer. Chest. 1994; 106(6 Suppl):337S–339S. PMID: 7988259.
Article6. Lima LN, da Silva RA, Gross JL, Deheinzelin D, Negri EM. Assessment of pulmonary function and quality of life in patients submitted to pulmonary resection for cancer. J Bras Pneumol. 2009; 35:521–528. PMID: 19618032.7. Manzano RM, Carvalho CR, Saraiva-Romanholo BM, Vieira JE. Chest physiotherapy during immediate postoperative period among patients undergoing upper abdominal surgery: randomized clinical trial. Sao Paulo Med J. 2008; 126:269–273. PMID: 19099160.
Article8. Win T, Groves AM, Ritchie AJ, Wells FC, Cafferty F, Laroche CM. The effect of lung resection on pulmonary function and exercise capacity in lung cancer patients. Respir Care. 2007; 52:720–726. PMID: 17521461.9. Funakoshi Y, Takeda S, Sawabata N, Okumura Y, Maeda H. Long-term pulmonary function after lobectomy for primary lung cancer. Asian Cardiovasc Thorac Ann. 2005; 13:311–315. PMID: 16304216.
Article10. Nomori H, Horio H, Fuyuno G, Kobayashi R, Yashima H. Respiratory muscle strength after lung resection with special reference to age and procedures of thoracotomy. Eur J Cardiothorac Surg. 1996; 10:352–358. PMID: 8737692.
Article11. Bott J, Blumenthal S, Buxton M, Ellum S, Falconer C, Garrod R, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax. 2009; 64(Suppl 1):i1–51. PMID: 19406863.
Article12. Hernandez Alava M, Wailoo A, Wolfe F, Michaud K. The relationship between EQ-5D, HAQ and pain in patients with rheumatoid arthritis. Rheumatology (Oxford). 2013; 52:944–950. PMID: 23339232.13. Novoa N, Varela G, Jimenez MF, Aranda JL. Influence of major pulmonary resection on postoperative daily ambulatory activity of the patients. Interact Cardiovasc Thorac Surg. 2009; 9:934–938. PMID: 19726452.
Article14. Miyoshi S, Yoshimasu T, Hirai T, Hirai I, Maebeya S, Bessho T, et al. Exercise capacity of thoracotomy patients in the early postoperative period. Chest. 2000; 118:384–390. PMID: 10936129.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative Management of Lung Resection Patients
- Validation of Prediction Models for Postoperative Pulmonary Complications after Lung Resection: A Retrospective Study
- The Effects of Self-Efficacy Promoting Pulmonary Rehabilitation Program in Out-Patients with Chronic Obstructive Pulmonary Disease
- Early Tailoring Thoracoplasty in Patients Undergoing Pulmonary Resection
- Nutritional Intake and Postoperative Pulmonary Complications among Lung Cancer Patients who Underwent Pulmonary Resection