Ann Rehabil Med.
2015 Dec;39(6):941-949. 10.5535/arm.2015.39.6.941.
Percutaneous Adhesiolysis Versus Transforaminal Epidural Steroid Injection for the Treatment of Chronic Radicular Pain Caused by Lumbar Foraminal Spinal Stenosis: A Retrospective Comparative Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. S3184@paik.ac.kr
- 2Department of Anesthesiology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Yonsei S Rehabilitation Clinic, Seoul, Korea.
- KMID: 2165620
- DOI: http://doi.org/10.5535/arm.2015.39.6.941
Abstract
OBJECTIVE
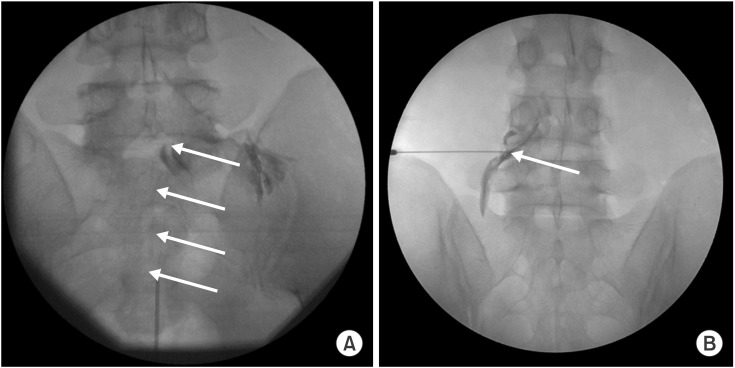
To investigate the efficacy of percutaneous adhesiolysis (PA) compared to fluoroscopy (FL)-guided transforaminal epidural steroid injection (TFESI) in patients with radicular pain caused by lumbar foraminal spinal stenosis (LFSS) by assessing pain relief and functional improvement at 4 and 12 weeks post-procedure.
METHODS
This retrospective study included 45 patients who underwent PA or FL-guided TFSEI for radicular pain caused by LFSS of at least 3 months' duration. Outcomes were assessed with the Oswestry Disability Index (ODI) and Verbal Numeric Pain Scale (VNS) before the procedure and at 4 and 12 weeks post-procedure. A successful outcome was defined by >50% improvement in the VNS score and >40% improvement in the ODI score.
RESULTS
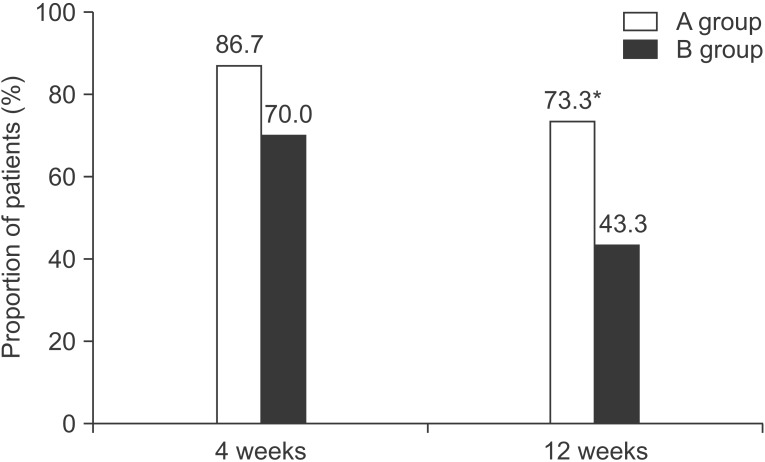
ODI and VNS scores improved 4 and 12 weeks post-procedure in both groups. Statistically significant differences between groups were observed in ODI and VNS at 12 weeks (p<0.05). The proportion of patients with successful outcomes was significantly different between the two groups only at the 12-week time point.
CONCLUSION
Our study suggests that PA is effective for pain reduction and functional improvement in patients with chronic radicular pain caused by LFSS. Therefore, PA can be considered for patients with previous ineffective responses to conservative treatment. Although PA seems to be more effective than TFEFI according to the results of our study, in order to fully elucidate the difference in effectiveness, a prospective study with a larger sample size is necessary.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Prognostic Value of Enhanced-MRI and Fluoroscopic Factors for Predicting the Effects of Transforaminal Steroid Injections on Lumbosacral Radiating Pain
Yun Suk Jung, Jee Hyun Suh, Ha Young Kim, Kyunghoon Min, Yoongul Oh, Donghwi Park, Ju Seok Ryu
Ann Rehabil Med. 2016;40(6):1071-1081. doi: 10.5535/arm.2016.40.6.1071.Lumbar foraminal neuropathy: an update on non-surgical management
Young Kook Choi
Korean J Pain. 2019;32(3):147-159. doi: 10.3344/kjp.2019.32.3.147.
Reference
-
1. Jenis LG, An HS. Spine update: lumbar foraminal stenosis. Spine (Phila Pa 1976). 2000; 25:389–394. PMID: 10703115.2. Kunogi J, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine (Phila Pa 1976). 1991; 16:1312–1320. PMID: 1750006.
Article3. Porter RW, Hibbert C, Evans C. The natural history of root entrapment syndrome. Spine (Phila Pa 1976). 1984; 9:418–421. PMID: 6236567.
Article4. Jinkins JR, Whittemore AR, Bradley WG. The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. AJR Am J Roentgenol. 1989; 152:1277–1289. PMID: 2718865.
Article5. Thomas E, Cyteval C, Abiad L, Picot MC, Taourel P, Blotman F. Efficacy of transforaminal versus interspinous corticosteroid injectionin discal radiculalgia: a prospective, randomised, double-blind study. Clin Rheumatol. 2003; 22:299–304. PMID: 14579160.6. Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000; 3:374–398. PMID: 16906179.
Article7. Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012; 15:E199–E245. PMID: 22622912.8. Kim SH, Choi WJ, Suh JH, Jeon SR, Hwang CJ, Koh WU, et al. Effects of transforaminal balloon treatment in patients with lumbar foraminal stenosis: a randomized, controlled, double-blind trial. Pain Physician. 2013; 16:213–224. PMID: 23703408.9. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998; 14:148–151. PMID: 9647457.
Article10. Smith CC, Booker T, Schaufele MK, Weiss P. Interlaminar versus transforaminal epidural steroid injections for the treatment of symptomatic lumbar spinal stenosis. Pain Med. 2010; 11:1511–1515. PMID: 20735751.
Article11. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis versus transforaminal epidural steroid injection in patients with postlumbar surgery syndrome. Reg Anesth Pain Med. 2014; 39:214–218. PMID: 24646624.
Article12. Chopra P, Smith HS, Deer TR, Bowman RC. Role of adhesiolysis in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 2005; 8:87–100. PMID: 16850047.13. Trescot AM, Chopra P, Abdi S, Datta S, Schultz DM. Systematic review of effectiveness and complications of adhesiolysis in the management of chronic spinal pain: an update. Pain Physician. 2007; 10:129–146. PMID: 17256027.14. Bogduk N. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain. 2009; 147:17–19. PMID: 19762151.
Article15. Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003; 3:310–316. PMID: 17166126.
Article16. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25:2940–2952. PMID: 11074683.
Article17. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial: Clinical Trial NCT00355914. Pain Physician. 2008; 11:121–132. PMID: 18354721.18. Lee JH, An JH, Lee SH. Comparison of the effectiveness of interlaminar and bilateral transforaminal epidural steroid injections in treatment of patients with lumbosacral disc herniation and spinal stenosis. Clin J Pain. 2009; 25:206–210. PMID: 19333170.
Article19. Kobayashi S, Takeno K, Miyazaki T, Kubota M, Shimada S, Yayama T, et al. Effects of arterial ischemia and venous congestion on the lumbar nerve root in dogs. J Orthop Res. 2008; 26:1533–1540. PMID: 18536056.
Article20. Cooper RG, Freemont AJ, Hoyland JA, Jenkins JP, West CG, Illingworth KJ, et al. Herniated intervertebral disc-associated periradicular fibrosis and vascular abnormalities occur without inflammatory cell infiltration. Spine (Phila Pa 1976). 1995; 20:591–598. PMID: 7604329.
Article21. Manchikanti L, Boswell MV, Rivera JJ, Pampati VS, Damron KS, McManus CD, et al. A randomized, controlled trial of spinal endoscopic adhesiolysis in chronic refractory low back and lower extremity pain [ISRCTN 16558617]. BMC Anesthesiol. 2005; 5:10. PMID: 16000173.
Article22. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15. PMID: 24478895.
Article23. Rabinovitch DL, Peliowski A, Furlan AD. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. 2009; 9:509–517. PMID: 19398387.
Article24. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E341–E354. PMID: 19935991.25. Manchikanti L, Pampati V, Fellows B, Rivera JJ, Damron KS, Beyer C, et al. Effectiveness of percutaneous adhesiolysis with hypertonic saline neurolysis in refractory spinal stenosis. Pain Physician. 2001; 4:366–373. PMID: 16902683.26. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis and predictive factors of treatment efficacy in patients with lumbosacral spinal stenosis. Pain Med. 2013; 14:1497–1504. PMID: 23802996.
Article27. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis using Navicath for the management of chronic pain due to lumbosacral disc herniation. Pain Physician. 2012; 15:213–221. PMID: 22622905.28. Rivest C, Katz JN, Ferrante FM, Jamison RN. Effects of epidural steroid injection on pain due to lumbar spinal stenosis or herniated disks: a prospective study. Arthritis Care Res. 1998; 11:291–297. PMID: 9791328.
Article29. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.30. Amundsen T, Weber H, Lilleas F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis Clinical and radiologic features. Spine (Phila Pa 1976). 1995; 20:1178–1186. PMID: 7638662.31. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am. 1990; 72:1178–1184. PMID: 2398088.
Article32. Park CH, Lee SH, Jung JY. Dural sac cross-sectional area does not correlate with efficacy of percutaneous adhesiolysis in single level lumbar spinal stenosis. Pain Physician. 2011; 14:377–382. PMID: 21785481.33. Choi E, Nahm FS, Lee PB. Evaluation of prognostic predictors of percutaneous adhesiolysis using a Racz catheter for post lumbar surgery syndrome or spinal stenosis. Pain Physician. 2013; 16:E531–E536. PMID: 24077203.34. Yousef AA, EL-Deen AS, Al-Deeb AE. The role of adding hyaluronidase to fluoroscopically guided caudal steroid and hypertonic saline injection in patients with failed back surgery syndrome: a prospective, double-blinded, randomized study. Pain Pract. 2010; 10:548–553. PMID: 20412501.
Article35. Kim SB, Lee KW, Lee JH, Kim MA, An BW. The effect of hyaluronidase in interlaminar lumbar epidural injection for failed back surgery syndrome. Ann Rehabil Med. 2012; 36:466–473. PMID: 22977771.
Article36. Kim SB, Lee KW, Lee JH, Kim MA, Kim BH. The additional effect of hyaluronidase in lumbar interlaminar epidural injection. Ann Rehabil Med. 2011; 35:405–411. PMID: 22506151.
Article37. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–140. PMID: 22430650.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Facet Joint Versus Transforaminal Epidural Steroid Injections in Patients With Cervical Radicular Pain due to Foraminal Stenosis: A Retrospective Comparative Study
- Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
- Selective Epidural Steroid Injection in a Patient with Refractory Radicular Leg Pain: A case report
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Oblique interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: A case report