Clin Endosc.
2011 Sep;44(1):22-26.
Comparison of Midazolam Alone versus Midazolam Plus Propofol during Endoscopic Submucosal Dissection
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. smpark@chungbuk.ac.kr
Abstract
- BACKGROUND/AIMS
For proper sedation during endoscopic submucosal dissection (ESD), propofol has been widely used. This study aimed to compare the levels of sedation and tolerance of patients treated with midazolam (M group) and a combination of midazolam and propofol (MP group) during ESD.
METHODS
A total of 44 consecutive patients undergoing ESD were randomly assigned to the two groups. In the M group, 2 mg of midazolam was given repeatedly to maintain after a loading dose of 5 mg. The MP group initially received 5 mg of midazolam and 20 mg of propofol. Then, we increased the dosage of propofol by 20 mg gradually.
RESULTS
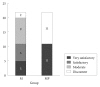
The average amount of midazolam was 12 mg in the M group. In the M group, 10 patients were given propofol additionally, since they failed to achieve proper sedation. The average amount of propofol was 181 mg in the MP group. Procedure time, vital signs and rates of complications were not significantly different between two groups. Movement of patients and discomfort were lower in the MP group.
CONCLUSIONS
During ESD, treatment with propofol and a low dose of midazolam for sedation provides greater satisfaction for endoscopists compared to midazolam alone.
Figure
Reference
-
1. Practice guidelines for sedation and analgesia by non-anesthesiologists. A report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Anesthesiology. 1996; 84:459–471. PMID: 8602682.2. Chokhavatia S, Nguyen L, Williams R, Kao J, Heavner JE. Sedation and analgesia for gastrointestinal endoscopy. Am J Gastroenterol. 1993; 88:393–396. PMID: 8094940.3. Gamble JA, Kawar P, Dundee JW, Moore J, Briggs LP. Evaluation of midazolam as an intravenous induction agent. Anaesthesia. 1981; 36:868–873. PMID: 7304889.
Article4. Al-Khudhairi D, Whitwam JG, McCloy RF. Midazolam and diazepam for gastroscopy. Anaesthesia. 1982; 37:1002–1006. PMID: 6127968.
Article5. Sebel PS, Lowdon JD. Propofol: a new intravenous anesthetic. Anesthesiology. 1989; 71:260–277. PMID: 2667401.6. Keeffe EB, O'Connor KW. 1989 A/S/G/E survey of endoscopic sedation and monitoring practices. Gastrointest Endosc. 1990; 36(3 Suppl):S13–S18. PMID: 2351253.7. Bell GD. Premedication, preparation, and surveillance. Endoscopy. 2000; 32:92–100. PMID: 10696836.
Article8. Carlsson U, Grattidge P. Sedation for upper gastrointestinal endoscopy: a comparative study of propofol and midazolam. Endoscopy. 1995; 27:240–243. PMID: 7664702.
Article9. Koo JS, Choi JH, Jung SW, et al. Conscious sedation with midazolam combined with propofol for colonoscopy. Korean J Gastrointest Endosc. 2007; 34:298–303.10. Jung M, Hofmann C, Kiesslich R, Brackertz A. Improved sedation in diagnostic and therapeutic ERCP: propofol is an alternative to midazolam. Endoscopy. 2000; 32:233–238. PMID: 10718389.
Article11. McClune S, McKay AC, Wright PM, Patterson CC, Clarke RS. Synergistic interaction between midazolam and propofol. Br J Anaesth. 1992; 69:240–245. PMID: 1389840.
Article12. Reimann FM, Samson U, Derad I, Fuchs M, Schiefer B, Stange EF. Synergistic sedation with low-dose midazolam and propofol for colonoscopies. Endoscopy. 2000; 32:239–244. PMID: 10718390.
Article13. Charlton JE. Monitoring and supplemental oxygen during endoscopy. BMJ. 1995; 310:886–887. PMID: 7719168.
Article14. Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002; 97:1159–1163. PMID: 12014721.
Article15. Cho H, Kim YM, Oh JH, et al. The effect of propofol for conscious sedation during colonoscopy: a prospective, randomized study. Korean J Med. 2005; 69:30–38.16. Kim MH, Doo YC, Yang SK, et al. The changes of SaO2 during upper endoscopy. Korean J Gastroenterol. 1990; 22:496–501.17. Steffes CP, Sugawa C, Wilson RF, Hayward SR. Oxygen saturation monitoring during endoscopy. Surg Endosc. 1990; 4:175–178. PMID: 2267651.
Article18. Cummings GC, Dixon J, Kay NH, et al. Dose requirements of ICI 35,868 (propofol, 'Diprivan') in a new formulation for induction of anaesthesia. Anaesthesia. 1984; 39:1168–1171. PMID: 6335003.
Article19. Choi WH, Kim SW, Lee YS, et al. The effect of upper gastrointestinal endoscopy using conscious sedation with propofol. Korean J Med. 2003; 64:509–515.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Noticement: Comparison of Midazolam Alone versus Midazolam Plus Propofol during Endoscopic Submucosal Dissection
- Safety and Efficacy of Deep Sedation with Propofol Alone or Combined with Midazolam Administrated by Nonanesthesiologist for Gastric Endoscopic Submucosal Dissection
- Harmony of Duet over Solo: Use of Midazolam or Propofol for Sedative Endoscopy in Pediatric Patients
- The Frequency of Apnea and Loss of Consciousness According to Propofol Dosage in Premedicated Patients with Midazolam
- Efficacy of Bispectral Index Monitoring for Midazolam and Meperidine Induced Sedation during Endoscopic Submucosal Dissection: A Prospective, Randomized Controlled Study