Clin Endosc.
2013 Nov;46(6):656-661.
Endoscopic Treatment of Duodenal Neuroendocrine Tumors
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. p1052ccy@hanmail.net
Abstract
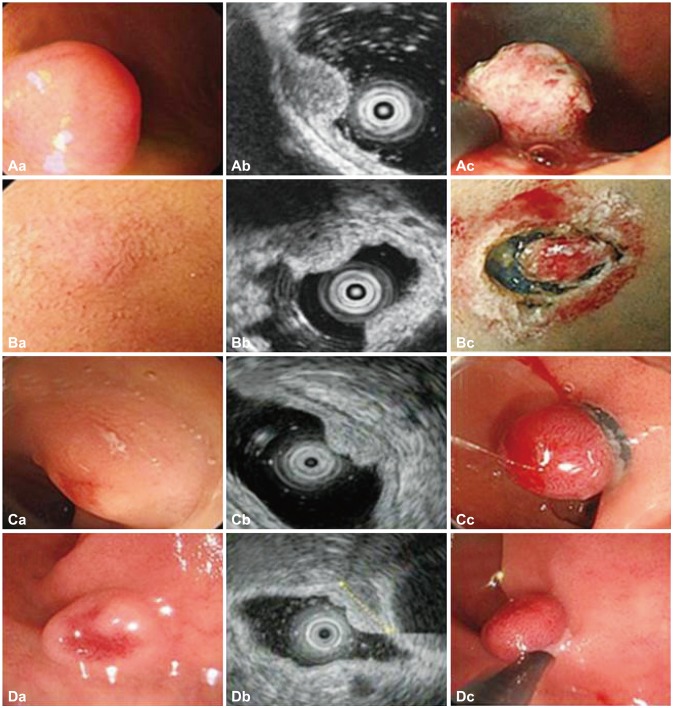
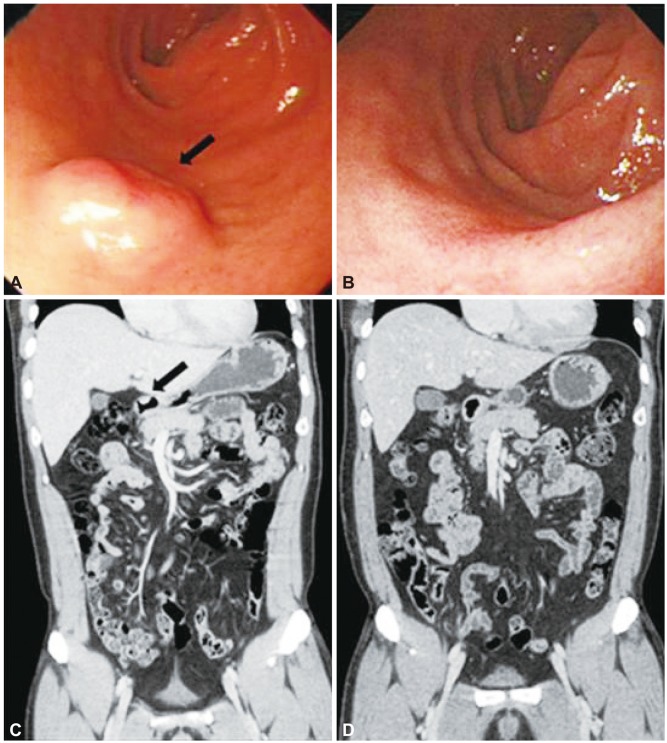
- Duodenal neuroendocrine tumors (NETs) are rare neoplasms. In this study, the medical records of 14 patients with duodenal NETs diagnosed at Chonnam National University Hospital from July 2001 to August 2011 were reviewed and analyzed retrospectively. Four patients were diagnosed in the first 5 years, and 10 patients were diagnosed in the latter 5 years of the study. Ten of 12 patients (83.3%) who underwent endoscopic biopsy were confirmed to have NET before resection. Endoscopic resection was performed in 12 patients, surgical resection in one patient, and regular follow-up in one patient who refused resection. None of the patients showed recurrence or distant metastasis. Duodenal NETs are increasingly observed and are mostly detected during screening upper gastrointestinal endoscopy. Careful endoscopic examination and biopsy can improve the diagnostic yield of NETs. Most well-differentiated, nonfunctional duodenal NETs that are limited to the mucosa/submucosa can be treated effectively with endoscopic resection.
MeSH Terms
Figure
Reference
-
1. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934–959. PMID: 12569593.
Article2. Burke AP, Sobin LH, Federspiel BH, Shekitka KM, Helwig EB. Carcinoid tumors of the duodenum. A clinicopathologic study of 99 cases. Arch Pathol Lab Med. 1990; 114:700–704. PMID: 1694655.4. Oberg K, Astrup L, Eriksson B, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine tumours (including bronchopulmonary and thymic neoplasms). Part I-general overview. Acta Oncol. 2004; 43:617–625. PMID: 15545182.5. Hedenbro JL, Ekelund M, Wetterberg P. Endoscopic diagnosis of submucosal gastric lesions. The results after routine endoscopy. Surg Endosc. 1991; 5:20–23. PMID: 1871670.6. Modlin IM, Shapiro MD, Kidd M, Eick G. Siegfried oberndorfer and the evolution of carcinoid disease. Arch Surg. 2007; 142:187–197. PMID: 17309971.
Article7. Modlin IM, Oberg K, Chung DC, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008; 9:61–72. PMID: 18177818.
Article8. Klöppel G, Heitz PU, Capella C, Solcia E. Pathology and nomenclature of human gastrointestinal neuroendocrine (carcinoid) tumors and related lesions. World J Surg. 1996; 20:132–141. PMID: 8661808.
Article9. Klöppel G, Rindi G, Anlauf M, Perren A, Komminoth P. Site-specific biology and pathology of gastroenteropancreatic neuroendocrine tumors. Virchows Arch. 2007; 451(Suppl 1):S9–S27. PMID: 17684761.
Article10. Rindi G, Klöppel G, Alhman H, et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006; 449:395–401. PMID: 16967267.
Article11. Hoffmann KM, Furukawa M, Jensen RT. Duodenal neuroendocrine tumors: classification, functional syndromes, diagnosis and medical treatment. Best Pract Res Clin Gastroenterol. 2005; 19:675–697. PMID: 16253893.
Article12. Kang BS, Kim JW. Gastrointestinal carcinoid tumor: clinical review of 36 cases. J Korean Surg Soc. 2009; 76:1–6.
Article13. Zimmer T, Scherübl H, Faiss S, Stölzel U, Riecken EO, Wiedenmann B. Endoscopic ultrasonography of neuroendocrine tumours. Digestion. 2000; 62(Suppl 1):45–50. PMID: 10940687.
Article14. Shimizu N, Kaminishi M. Management of patients with neuroendocrine tumors of the esophagus, stomach, and duodenum. Nihon Geka Gakkai Zasshi. 2008; 109:147–151. PMID: 18536318.15. Deacon AC. The measurement of 5-hydroxyindoleacetic acid in urine. Ann Clin Biochem. 1994; 31(Pt 3):215–232. PMID: 7520678.
Article16. Eriksson B, Klöppel G, Krenning E, et al. Consensus guidelines for the management of patients with digestive neuroendocrine tumors: well-differentiated jejunal-ileal tumor/carcinoma. Neuroendocrinology. 2008; 87:8–19. PMID: 18097129.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Treatment of Gastric and Duodenal Neuroendocrine Tumors: Present and Future
- Two Cases of Endoscopic Papillectomy for Neuroendocrine Tumor Arising from Minor Papilla
- Endoscopic Papillectomy for Synchronous Major and Minor Duodenal Papilla Neuroendocrine Tumors
- Duodenal Neuroendocrine Tumor: a Diagnostic Surprise during Workup for Anemia
- Successful Endoscopic Submucosal Dissection Using Open Peroral Endoscopic Myotomy for Duodenal Neuroendocrine Tumor