Clin Endosc.
2013 Nov;46(6):637-642.
Late Complications and Stone Recurrence Rates after Bile Duct Stone Removal by Endoscopic Sphincterotomy and Large Balloon Dilation are Similar to Those after Endoscopic Sphincterotomy Alone
- Affiliations
-
- 1Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. jmhan@cu.ac.kr
Abstract
- BACKGROUND/AIMS
Between endoscopic sphincterotomy (ES) alone and combined endoscopic sphincterotomy and large balloon dilation (ES-LBD) groups, efficacy and long-term complications, difference in biliary stone recurrence rate, and risk factors of stone recurrence were compared.
METHODS
Medical records of 222 patients who underwent ERCP for biliary stone removal were retrospectively reviewed. Patients with dilated CBD > or =11 mm and follow-up longer than 6 months were included.
RESULTS
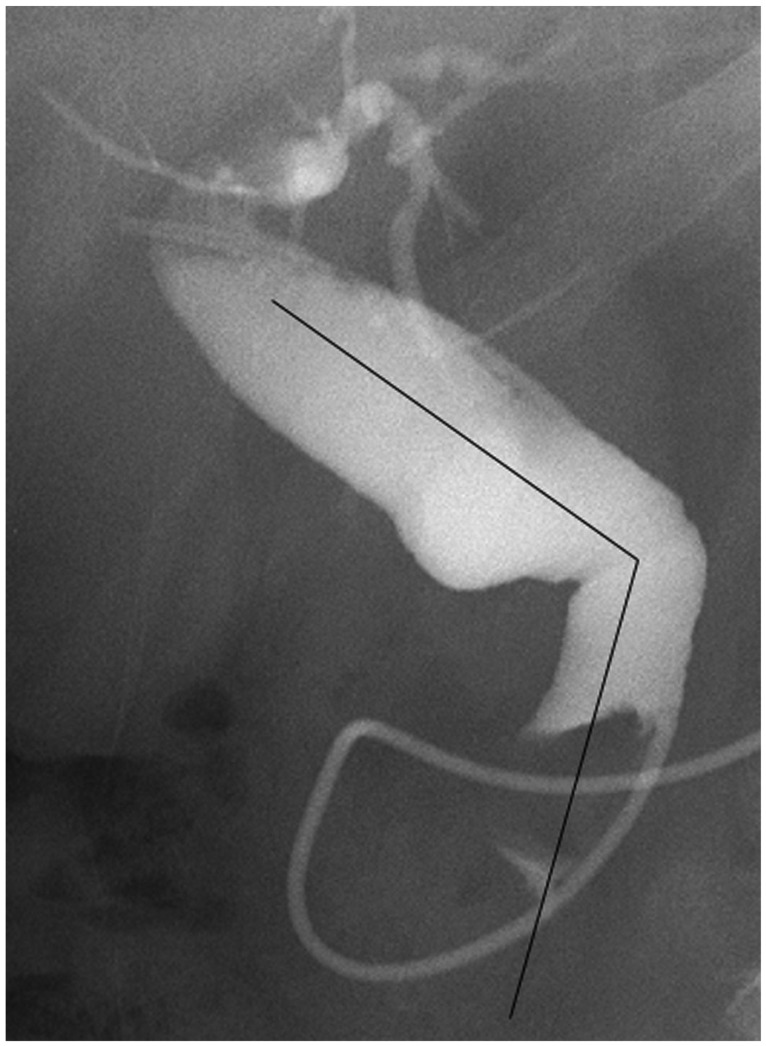
There were 101 patients in ES-LBD group and 121 patients in ES group. Mean follow-up duration was 25.0 (6-48) months and 13.0 (6-43) months, respectively (p=0.001). There was no difference in number of ERCP sessions, brown pigment stones, angle between mid and distal common bile duct (CBD angle) <135degrees, and lithotripsy rate. Complete retrieval success rate was excellent in both groups (100% vs. 99%). Early complication rate of ES-LBD and ES alone group was 4 and 4.1%, respectively (p=1.000). One patient in ES-LBD group died from delayed bleeding. Late complication rate was 5.9 and 3.3%, respectively (p=1.000). Stone recurrence rate was 6.9% and 5.8%, respectively (p=0.984). The only Independent risk factor of stone recurrence was presence of periampullary diverticulum.
CONCLUSIONS
Late complication and stone recurrence rates were similar between ES-LBD and ES alone groups.
Keyword
MeSH Terms
Figure
Reference
-
1. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003; 57:156–159. PMID: 12556775.
Article2. Stefanidis G, Viazis N, Pleskow D, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011; 106:278–285. PMID: 21045816.
Article3. Youn YH, Lim HC, Jahng JH, et al. The increase in balloon size to over 15 mm does not affect the development of pancreatitis after endoscopic papillary large balloon dilatation for bile duct stone removal. Dig Dis Sci. 2011; 56:1572–1577. PMID: 20945093.4. Yasuda I, Fujita N, Maguchi H, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010; 72:1185–1191. PMID: 20869711.
Article5. Ohashi A, Tamada K, Wada S, et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009; 21:73–77. PMID: 19691777.
Article6. Hisatomi K, Ohno A, Tabei K, Kubota K, Matsuhashi N. Effects of large-balloon dilation on the major duodenal papilla and the lower bile duct: histological evaluation by using an ex vivo adult porcine model. Gastrointest Endosc. 2010; 72:366–372. PMID: 20674625.
Article7. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.
Article8. Kim HJ, Choi HS, Park JH, et al. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007; 66:1154–1160. PMID: 17945223.
Article9. Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001; 49:686–691. PMID: 11600473.
Article10. Sato H, Kodama T, Takaaki J, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut. 1997; 41:541–544. PMID: 9391256.
Article11. Tsujino T, Isayama H, Ito Y, et al. Long-term outcomes (mean follow-up period > 10 years) of endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2008; 67:AB163–AB164.12. Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006; 20:1594–1599. PMID: 16858527.
Article13. Ueno N, Ozawa Y, Aizawa T. Prognostic factors for recurrence of bile duct stones after endoscopic treatment by sphincter dilation. Gastrointest Endosc. 2003; 58:336–340. PMID: 14528204.
Article14. Kojima Y, Nakagawa H, Miyata A, et al. Long-term prognosis of bile duct stones: endoscopic papillary balloon dilatation versus endoscopic sphincterotomy. Dig Endosc. 2010; 22:21–24. PMID: 20078660.
Article15. Tsujino T, Kawabe T, Komatsu Y, et al. Endoscopic papillary balloon dilation for bile duct stone: immediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007; 5:130–137. PMID: 17234559.16. Lee JH. Is combination biliary sphincterotomy and balloon dilation a better option than either alone in endoscopic removal of large bileduct stones? Gastrointest Endosc. 2007; 66:727–729. PMID: 17905014.
Article17. Keizman D, Ish Shalom M, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006; 64:60–65. PMID: 16813804.
Article18. Yasuda I. Management of the bile duct stone: current situation in Japan. Dig Endosc. 2010; 22(Suppl 1):S76–S78. PMID: 20590777.
Article19. Kim KH, Rhu JH, Kim TN. Recurrence of bile duct stones after endoscopic papillary large balloon dilation combined with limited sphincterotomy: long-term follow-up study. Gut Liver. 2012; 6:107–112. PMID: 22375179.
Article20. Ang TL, Teo EK, Fock KM, Lyn Tan JY. Are there roles for intraductal US and saline solution irrigation in ensuring complete clearance of common bile duct stones? Gastrointest Endosc. 2009; 69:1276–1281. PMID: 19249039.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Papillary Balloon Dilation/Endoscopic Papillary Large Balloon Dilation
- Endoscopic Sphincterotomy, Balloon Stone Extraction, and Basket Stone Extraction
- Endoscopic Removal of Bile Duct Stones
- Recurrence of Bile Duct Stones after Endoscopic Papillary Large Balloon Dilation Combined with Limited Sphincterotomy: Long-Term Follow-Up Study
- Recurrent Common Bile Duct Stone and Endoscopic Treatment after Endoscopic Papillary Large Balloon Dilatation with Minor Endoscopic Sphincterotomy