Clin Endosc.
2013 Nov;46(6):627-632.
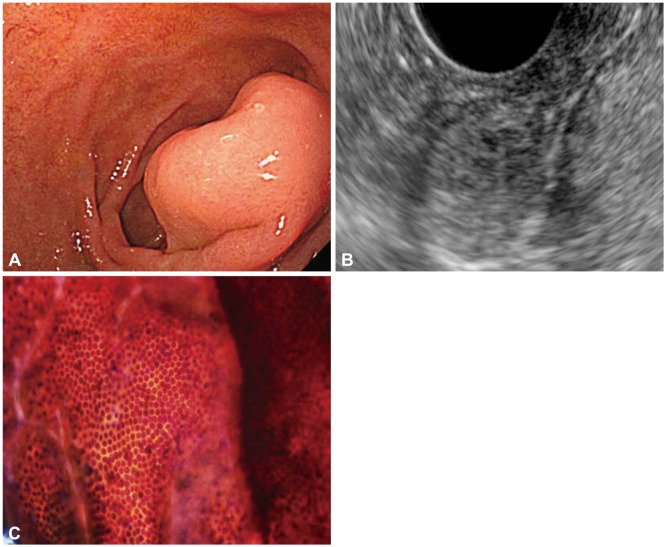
Performance and Clinical Role of Endoscopic Ultrasound Fine Needle Aspiration for Diagnosing Gastrointestinal Intramural Lesions
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. ykcho@catholic.ac.kr
Abstract
- BACKGROUND/AIMS
We evaluated the performance, clinical role, and diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) in gastrointestinal intramural lesions.
METHODS
Procedural and pathologic data were reviewed from consecutive patients undergoing EUS-FNA for intramural lesions. Final diagnoses were determined by surgical histopathologic conformation and the diagnosis of malignancy, including clinical follow-up with repeat imaging.
RESULTS
Forty-six patients (mean age, 47 years; 24 males) underwent EUS-FNA. Lesions were located in the stomach (n=31), esophagus (n=5), and duodenum (n=10). The median lesion size was 2 cm (range, 1 to 20.6). Final diagnoses were obtained in 22 patients (48%). EUS-FNA was diagnostic in 40 patients (87%). The diagnostic accuracy of cytology for differentiating between benign and malignant lesions was 82%; diagnostic error occurred in three patients (6%). The cytologic results influenced clinical judgment in 78% cases. The primary reasons for negative or no clinical impact were false-negative results, misdirected patient management, and inconclusive cytology.
CONCLUSIONS
EUS-FNA exhibited an 87% diagnostic yield for gastrointestinal intramural lesions; the accuracy of cytology for differentiating malignancy was 82%. The limitations of EUS-FNA were primarily because of nondiagnostic sampling (9%) and probable diagnostic error (6%); these factors may influence the clinical role of EUS-FNA.
Keyword
MeSH Terms
Figure
Reference
-
1. Hwang JH, Saunders MD, Rulyak SJ, Shaw S, Nietsch H, Kimmey MB. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005; 62:202–208. PMID: 16046979.
Article2. Karaca C, Turner BG, Cizginer S, Forcione D, Brugge W. Accuracy of EUS in the evaluation of small gastric subepithelial lesions. Gastrointest Endosc. 2010; 71:722–727. PMID: 20171632.
Article3. Ha CY, Shah R, Chen J, Azar RR, Edmundowicz SA, Early DS. Diagnosis and management of GI stromal tumors by EUS-FNA: a survey of opinions and practices of endosonographers. Gastrointest Endosc. 2009; 69:1039–1044. PMID: 19410040.
Article4. Wiersema MJ, Hawes RH, Tao LC, et al. Endoscopic ultrasonography as an adjunct to fine needle aspiration cytology of the upper and lower gastrointestinal tract. Gastrointest Endosc. 1992; 38:35–39. PMID: 1612376.
Article5. Matsui M, Goto H, Niwa Y, Arisawa T, Hirooka Y, Hayakawa T. Preliminary results of fine needle aspiration biopsy histology in upper gastrointestinal submucosal tumors. Endoscopy. 1998; 30:750–755. PMID: 9932753.
Article6. Ando N, Goto H, Niwa Y, et al. The diagnosis of GI stromal tumors with EUS-guided fine needle aspiration with immunohistochemical analysis. Gastrointest Endosc. 2002; 55:37–43. PMID: 11756912.
Article7. Chen VK, Eloubeidi MA. Endoscopic ultrasound-guided fine-needle aspiration of intramural and extraintestinal mass lesions: diagnostic accuracy, complication assessment, and impact on management. Endoscopy. 2005; 37:984–989. PMID: 16189771.
Article8. Eltoum IA, Chhieng DC, Jhala D, et al. Cumulative sum procedure in evaluation of EUS-guided FNA cytology: the learning curve and diagnostic performance beyond sensitivity and specificity. Cytopathology. 2007; 18:143–150. PMID: 17388936.
Article9. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002; 33:459–465. PMID: 12094370.
Article10. Mekky MA, Yamao K, Sawaki A, et al. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010; 71:913–919. PMID: 20226456.
Article11. Watson RR, Binmoeller KF, Hamerski CM, et al. Yield and performance characteristics of endoscopic ultrasound-guided fine needle aspiration for diagnosing upper GI tract stromal tumors. Dig Dis Sci. 2011; 56:1757–1762. PMID: 21360279.
Article12. Hoda KM, Rodriguez SA, Faigel DO. EUS-guided sampling of suspected GI stromal tumors. Gastrointest Endosc. 2009; 69:1218–1223. PMID: 19394006.
Article13. Philipper M, Hollerbach S, Gabbert HE, et al. Prospective comparison of endoscopic ultrasound-guided fine-needle aspiration and surgical histology in upper gastrointestinal submucosal tumors. Endoscopy. 2010; 42:300–305. PMID: 20306384.
Article14. Demetri GD, Benjamin RS, Blanke CD, et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST): update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw. 2007; 5(Suppl 2):S1–S29. PMID: 17624289.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- How to optimize the diagnostic yield of endoscopic ultrasoundguided fine-needle sampling in solid pancreatic lesions from a technical perspective
- How Can We Get the Best Results with Endoscopic Ultrasound-Guided Fine Needle Aspiration?
- Review of the 2017 European Society of Gastrointestinal Endoscopy Guidelines for Endoscopic Ultrasound - Guided Sampling in Pancreaticobiliary Lesions