Brain Tumor Res Treat.
2016 Apr;4(1):8-12. 10.14791/btrt.2016.4.1.8.
Hemangiopericytoma of the Cerebellopontine Angle: A Wolf in Sheep's Clothing
- Affiliations
-
- 1Department of Neurosurgery, Fattouma Bourguiba University Hospital, University of Medicine of Monastir, Monastir, Tunisia. atefbn@hotmail.fr
- 2Department of Neurosurgery, Ben Arous Trauma Center, University of Medicine of Tunis El Manar, Tunis, Tunisia.
- 3Department of Pathology, La Rabta University Hospital, University of Medicine Tunis El Manar, Tunis, Tunisia.
- 4Department of Neurosurgery, The Tunisian National Institute of Neurology, University of Medicine of Tunis El Manar, Tunis, Tunisia.
- KMID: 2165227
- DOI: http://doi.org/10.14791/btrt.2016.4.1.8
Abstract
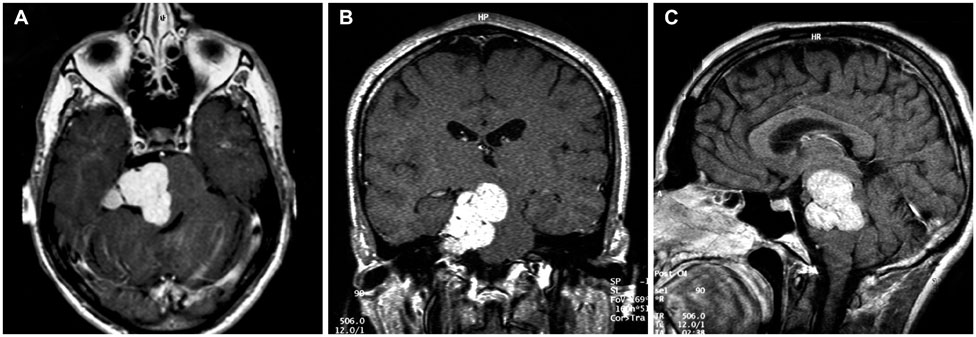
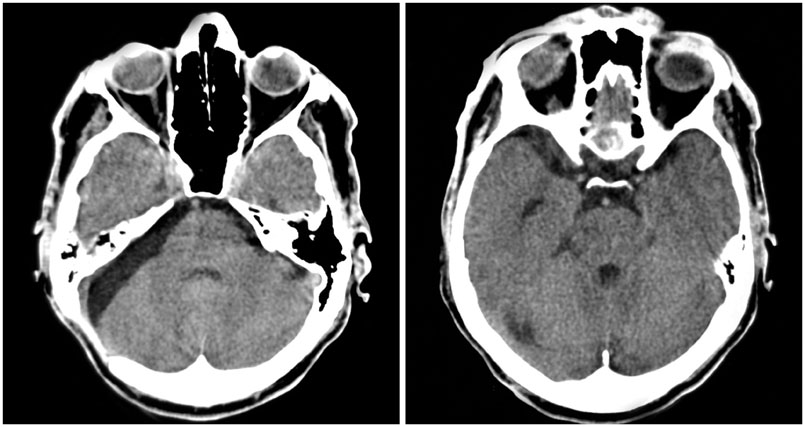
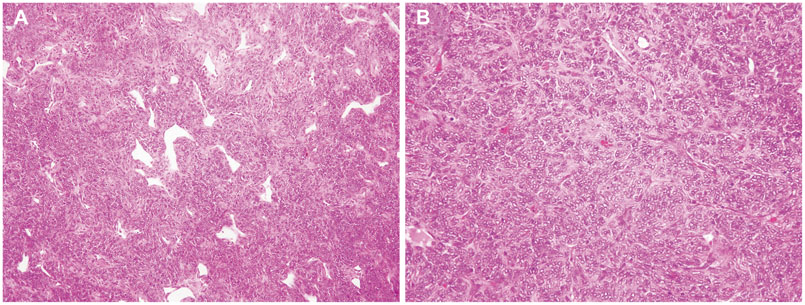
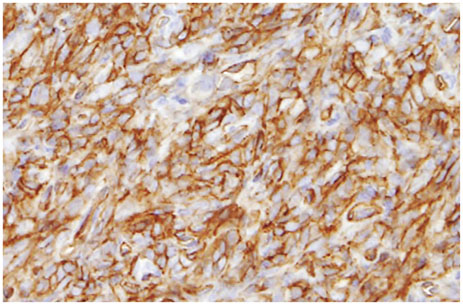
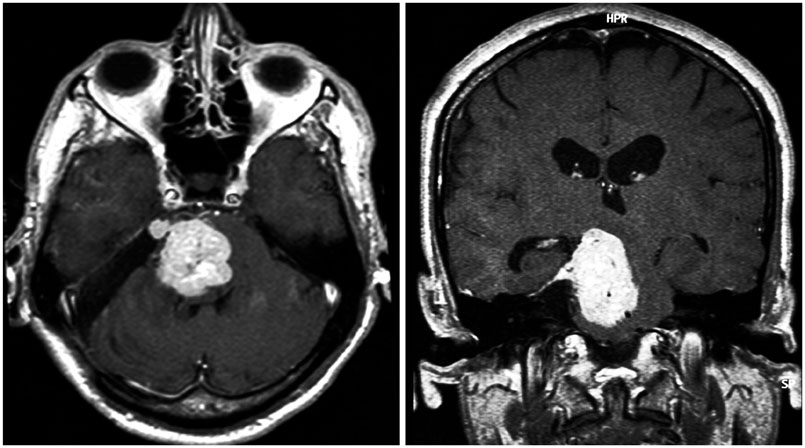
- Primary meningeal hemangiopericytoma (HPC) is a rare, aggressive dura based tumor that remarkably mimics a meningioma clinically and radiologically. Its occurrence within the cerebellopontine angle (CPA) is exceptional, and establishing the exact diagnosis is of the utmost importance since total resection remains the cornerstone of treatment. A 42-year-old man presented with a three-month history of progressively worsening vertigo and difficulty in walking. On admission, his neurological examination revealed a right peripheral facial palsy, right abducens palsy and left hemiparesis, suggesting the diagnosis of Millard-Gubler syndrome. Computed tomography and magnetic resonance imaging demonstrated a homogeneously enhancing dura based lesion of the right CPA causing major brain stem compression. There was no widening of the ipsilateral internal auditory canal. A standard retrosigmoid craniotomy was performed to access the right CPA. Exposure of the lesion revealed a well-encapsulated, gray, fibrous lesion, which appeared to originate from the tentorium. Gross total resection was achieved and confirmed radiologically. The microscopic features and the immunohistochemical profile confirmed the diagnosis of a HPC, and adjuvant radiation therapy was administered. Ten years later, the patient presented with a severe neurological deficit due to a local recurrence, but at that time refused any second intervention. He died three months later. HPC can locate within the CPA and present as a Millard-Gubler syndrome. The diagnosis should be kept in mind in case of a CPA dura based tumor. Radical surgery plus radiation therapy can maximize the recurrence-free survival and close follow-up remains mandatory to spot recurrences early.
MeSH Terms
Figure
Reference
-
1. Kumar N, Kumar R, Kapoor R, et al. Intracranial meningeal hemangiopericytoma: 10 years experience of a tertiary care Institute. Acta Neurochir (Wien). 2012; 154:1647–1651.
Article2. Molnar P, Nemes Z. Hemangiopericytoma of the cerebello-pontine angle. Diagnostic pitfalls and the diagnostic value of the subunit A of factor XIII as a tumor marker. Clin Neuropathol. 1995; 14:19–24.3. Mallucci CL, Ward V, Carney AS, O'Donoghue GM, Robertson I. Clinical features and outcomes in patients with non-acoustic cerebellopontine angle tumours. J Neurol Neurosurg Psychiatry. 1999; 66:768–771.
Article4. Alén JF, Lobato RD, Gómez PA, et al. Intracranial hemangiopericytoma: study of 12 cases. Acta Neurochir (Wien). 2001; 143:575–586.
Article5. Tashjian VS, Khanlou N, Vinters HV, Canalis RF, Becker DP. Hemangiopericytoma of the cerebellopontine angle: a case report and review of the literature. Surg Neurol. 2009; 72:290–295.
Article6. Cho JM, Kim SH, Kim SH, Lee KS, Chang JH. Recurred cerebellopontine angle haemangiopericytoma 5 years after stereotactic radiosurgery. Clin Neurol Neurosurg. 2011; 113:931–933.
Article7. Zeng J, Ogera P, Benardete EA, Nicastri AD, Rao C. Cellular solitary fibrous tumor (hemangiopericytoma) with anaplasia at cerebellopontine angle--a case report. Pathol Res Pract. 2012; 208:493–496.
Article8. Salunke P, Futane S, Gupta K, Vasishta RK. Cerebello-pontine angle hemangiopericytoma: an orphan differential diagnosis. Clin Neurol Neurosurg. 2013; 115:1184–1186.
Article9. Teoh JW, Goh BS, Shahizon Azura MM, Siti Aishah MA, Nor Hafliza MS. An unexpected lesion in cerebellopontine angle: hemangiopericytoma. Med J Malaysia. 2014; 69:146–147.10. Melone AG, D'Elia A, Santoro F, et al. Intracranial hemangiopericytoma--our experience in 30 years: a series of 43 cases and review of the literature. World Neurosurg. 2014; 81:556–562.
Article11. Soyuer S, Chang EL, Selek U, McCutcheon IE, Maor MH. Intracranial meningeal hemangiopericytoma: the role of radiotherapy: report of 29 cases and review of the literature. Cancer. 2004; 100:1491–1497.
Article12. Zhou JL, Liu JL, Zhang J, Zhang M. Thirty-nine cases of intracranial hemangiopericytoma and anaplastic hemangiopericytoma: a retrospective review of MRI features and pathological findings. Eur J Radiol. 2012; 81:3504–3510.
Article13. Liu L, Yin B, Geng DY, Li Y, Zhang BY, Peng WJ. Comparison of ADC values of intracranial hemangiopericytomas and angiomatous and anaplastic meningiomas. J Neuroradiol. 2014; 41:188–194.
Article14. Chen H, Zeng XW, Wu JS, et al. Solitary fibrous tumor of the central nervous system: a clinicopathologic study of 24 cases. Acta Neurochir (Wien). 2012; 154:237–248. discussion 248.
Article15. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.
Article16. Erdag G, Qureshi HS, Patterson JW, Wick MR. Solitary fibrous tumors of the skin: a clinicopathologic study of 10 cases and review of the literature. J Cutan Pathol. 2007; 34:844–850.
Article17. Chamberlain MC, Glantz MJ. Sequential salvage chemotherapy for recurrent intracranial hemangiopericytoma. Neurosurgery. 2008; 63:720–726. author reply 726-7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebellopontine Angle Medulloblastoma: Case Report
- Four Cases of Large Cerebellopontine Angle Tumors Removed by Translabyrinthine Approach
- A Case of Parasitic Cyst from Sparganosis in the Cerebellopontine Angle
- Cystic Trigeminal Neurinoma at Cerebellopontine Angle
- A Case of Right Cerebellopontine-Angle Lesion: Psychotic Symptoms and Magnetic Resonance Imaging Findings