J Bone Metab.
2016 May;23(2):85-93. 10.11005/jbm.2016.23.2.85.
Difference in Bone Mineral Density Change at the Lateral Femoral Cortices according to Administration of Different Bisphosphonate Agents
- Affiliations
-
- 1Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Biomedical Science, School of Medicine, Kyungpook National University, Daegu, Korea.
- 3Biostatistics Collaboration Lab, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Orthopaedic Surgery, Kyungpook National University Hospital, Daegu, Korea. ihpark@knu.ac.kr
- 5Department of Orthopedic Surgery, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea. kyang@yuhs.ac
- 6Department of Policy Research Affairs, National Health Insurance Service, Ilsan Hospital, Goyang, Korea.
- KMID: 2165122
- DOI: http://doi.org/10.11005/jbm.2016.23.2.85
Abstract
- BACKGROUND
To retrospectively assess whether the response of subtrochanteric lateral cortex (STLC) is different according to the bisphosphonate agents in terms of bone mineral density (BMD) change.
METHODS
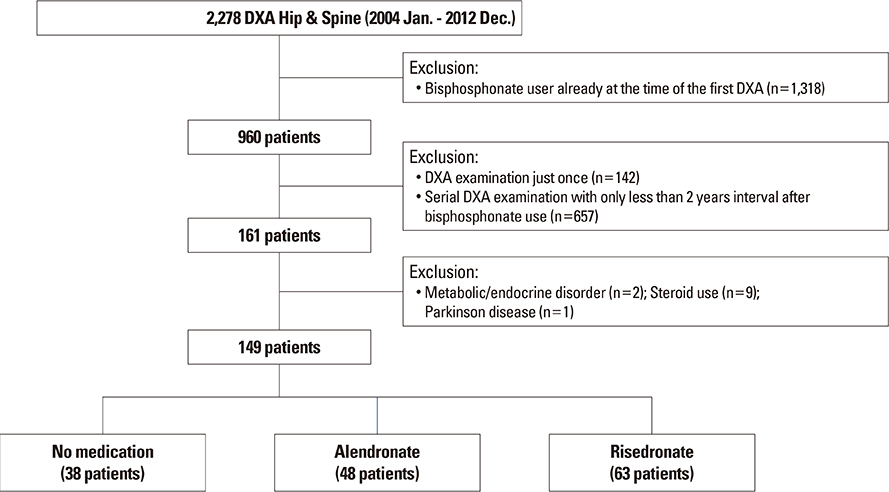
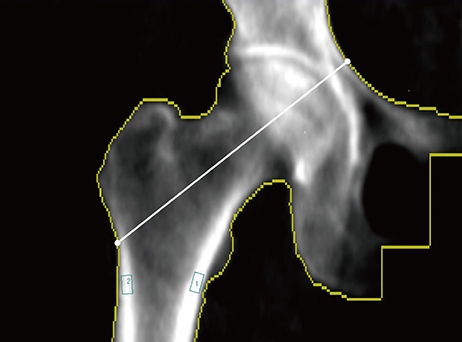
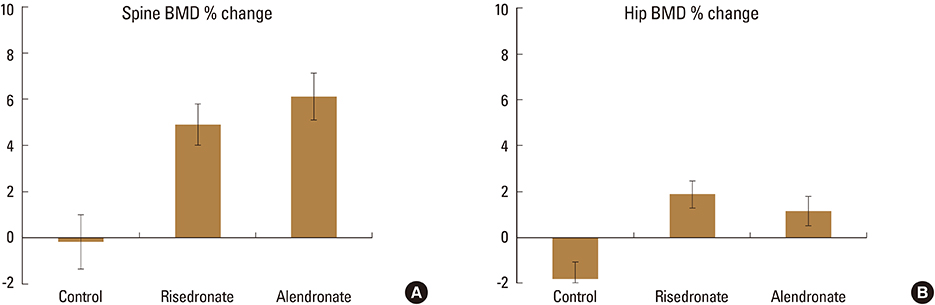
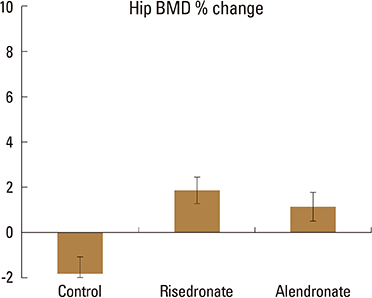
A total of 149 subjects, who had 2- to 4-year interval follow-up of BMD using dual energy X-ray absorptiometry (DXA), were included in this retrospective study divided into following 3 groups: control group (no consumption of any anti-osteoporotic drugs, n=38), alendronate group (naïve alendronate users, n=48), risedronate group (naïve risedronate users, n=63). BMD was measured at the STLC and subtrochanteric medial cortex (STMC) in each patient by drawing rectangular ROIs at the bone cortices. The percent change of BMD at the STLC were compared between the aforementioned 3 groups by using analysis of covariance model to control five independent variables of age, body mass index, percent change of STMC, hip axis length, time interval between DXA examinations.
RESULTS
The least square mean values±standard deviation of the percent change of BMD in the control, alendronate, and risedronate groups were 1.46±1.50, 2.23±1.26, and 6.96±1.11, respectively. The risedronate group showed significantly higher change of BMD percentage compared with the control (adjusted P=0.012) or alendronate (adjusted P=0.016) groups.
CONCLUSIONS
The percent change of BMD at the STLC in the risedronate user group was greater than the alendronate and control groups. The implication of these changes needs to be further verified.
Keyword
MeSH Terms
Figure
Reference
-
1. Bone HG, Hosking D, Devogelaer JP, et al. Ten years' experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004; 350:1189–1199.
Article2. Dell RM, Adams AL, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res. 2012; 27:2544–2550.
Article3. Goh SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg Br. 2007; 89:349–353.4. Lee YK, Ha YC, Park C, et al. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013; 24:707–711.
Article5. Meier RP, Perneger TV, Stern R, et al. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med. 2012; 172:930–936.
Article6. Schilcher J, Koeppen V, Aspenberg P, et al. Risk of atypical femoral fracture during and after bisphosphonate use. Acta Orthop. 2015; 86:100–107.
Article7. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011; 364:1728–1737.
Article8. Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996-2007. J Bone Miner Res. 2011; 26:553–560.
Article9. Franceschetti P, Bondanelli M, Caruso G, et al. Risk factors for development of atypical femoral fractures in patients on long-term oral bisphosphonate therapy. Bone. 2013; 56:426–431.
Article10. Odvina CV, Zerwekh JE, Rao DS, et al. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005; 90:1294–1301.
Article11. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.
Article12. Yang KH, Won JH, Yoon HK, et al. High concentrations of pamidronate in bone weaken the mechanical properties of intact femora in a rat model. Yonsei Med J. 2007; 48:653–658.
Article13. Duda GN, Heller M, Albinger J, et al. Influence of muscle forces on femoral strain distribution. J Biomech. 1998; 31:841–846.
Article14. Russell RG, Watts NB, Ebetino FH, et al. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. 2008; 19:733–759.
Article15. Edwards BJ, Bunta AD, Lane J, et al. Bisphosphonates and nonhealing femoral fractures: analysis of the FDA Adverse Event Reporting System (FAERS) and international safety efforts: a systematic review from the Research on Adverse Drug Events And Reports (RADAR) project. J Bone Joint Surg Am. 2013; 95:297–307.
Article16. Baim S, Wilson CR, Lewiecki EM, et al. Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom. 2005; 8:371–378.
Article17. Reid DM, Hosking D, Kendler D, et al. A comparison of the effect of alendronate and risedronate on bone mineral density in postmenopausal women with osteoporosis: 24-month results from FACTS-International. Int J Clin Pract. 2008; 62:575–584.
Article18. Yano T, Yamada M, Konda T, et al. Risedronate improves bone architecture and strength faster than alendronate in ovariectomized rats on a low-calcium diet. J Bone Miner Metab. 2014; 32:653–659.
Article19. Koeppen VA, Schilcher J, Aspenberg P. Atypical fractures do not have a thicker cortex. Osteoporos Int. 2012; 23:2893–2896.
Article20. Napoli N, Jin J, Peters K, et al. Are women with thicker cortices in the femoral shaft at higher risk of subtrochanteric/diaphyseal fractures? The study of osteoporotic fractures. J Clin Endocrinol Metab. 2012; 97:2414–2422.
Article21. Unnanuntana A, Ashfaq K, Ton QV, et al. The effect of long-term alendronate treatment on cortical thickness of the proximal femur. Clin Orthop Relat Res. 2012; 470:291–298.
Article22. Ebetino FH, Hogan AM, Sun S, et al. The relationship between the chemistry and biological activity of the bisphosphonates. Bone. 2011; 49:20–33.
Article23. Roelofs AJ, Stewart CA, Sun S, et al. Influence of bone affinity on the skeletal distribution of fluorescently labeled bisphosphonates in vivo. J Bone Miner Res. 2012; 27:835–847.
Article24. Turek J, Ebetino FH, Lundy MW, et al. Bisphosphonate binding affinity affects drug distribution in both intracortical and trabecular bone of rabbits. Calcif Tissue Int. 2012; 90:202–210.
Article25. Bala Y, Depalle B, Farlay D, et al. Bone micromechanical properties are compromised during long-term alendronate therapy independently of mineralization. J Bone Miner Res. 2012; 27:825–834.
Article26. Burr DB, Diab T, Koivunemi A, et al. Effects of 1 to 3 years' treatment with alendronate on mechanical properties of the femoral shaft in a canine model: implications for subtrochanteric femoral fracture risk. J Orthop Res. 2009; 27:1288–1292.
Article27. Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010; 25:2267–2294.
Article28. Cheon SH, Oh CW, Lee JY, et al. Early diagnosis of impending femoral insufficiency fractures by use of MRI: case report and review of the literature. J Orthop Sci. 2013; 18:843–848.
Article29. Kim S, Yang KH, Lim H, et al. Detection of prefracture hip lesions in atypical subtrochanteric fracture with dual-energy x-ray absorptiometry images. Radiology. 2014; 270:487–495.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a 'Drug Holiday' on Bone Mineral Density and Bone Turnover Marker During Bisphosphonate Therapy
- The relationship between grip strength and femoral and vertebral bone mineral density in peri-and postmenopausal women
- Effects of Body Composition, Leptin, and Adiponectin on Bone Mineral Density in Prepubertal Girls
- Comparison of Femoral Morphology and Bone Mineral Density between Femoral Neck Fractures and Trochanteric Fractures in 65+ Females
- Atypical Subtrochanteric and Diaphyseal Femoral Fractures