Clin Exp Otorhinolaryngol.
2016 Jun;9(2):136-142. 10.21053/ceo.2015.00584.
Immediate and Sustained Improvement in Behavior and Life Quality by Adenotonsillectomy in Children With Sleep-Disordered Breathing
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea. binent@hanmail.net
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Otolaryngology-Head and Neck Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 5Division of Child and Adolescent Psychiatry, Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Dermatology, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- KMID: 2165056
- DOI: http://doi.org/10.21053/ceo.2015.00584
Abstract
OBJECTIVES
To investigate longitudinal changes in behavior and quality-of-life (QoL) in children with sleep disordered breathing (SDB) after adenotonsillectomy (AT).
METHODS
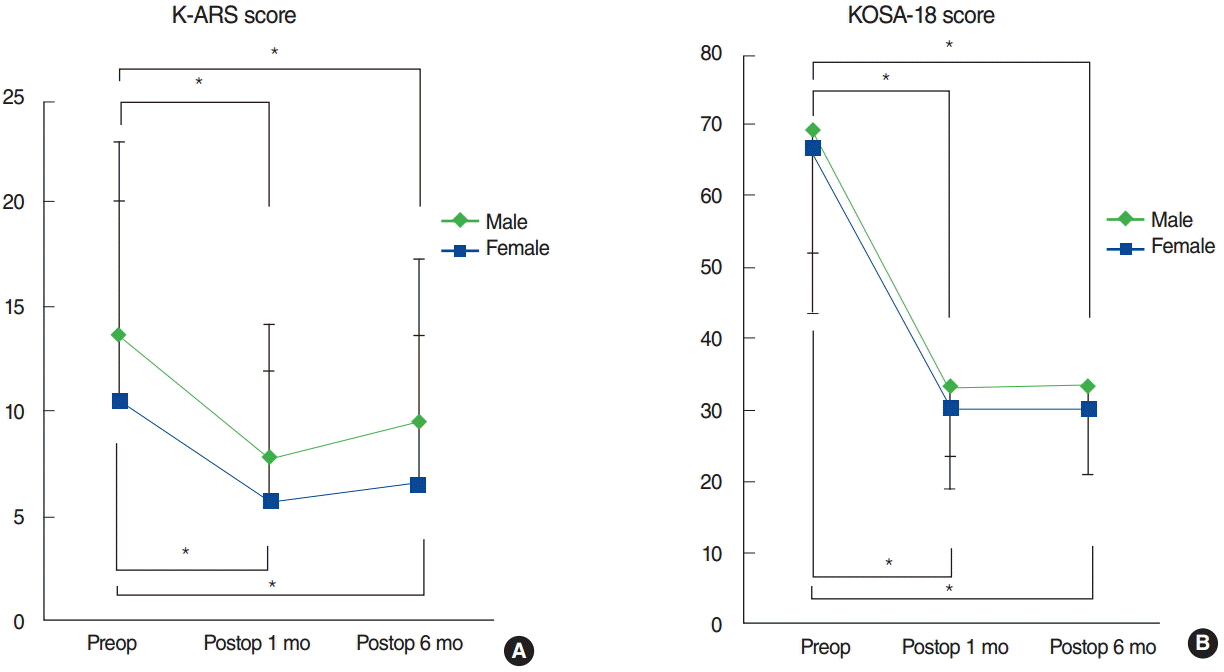
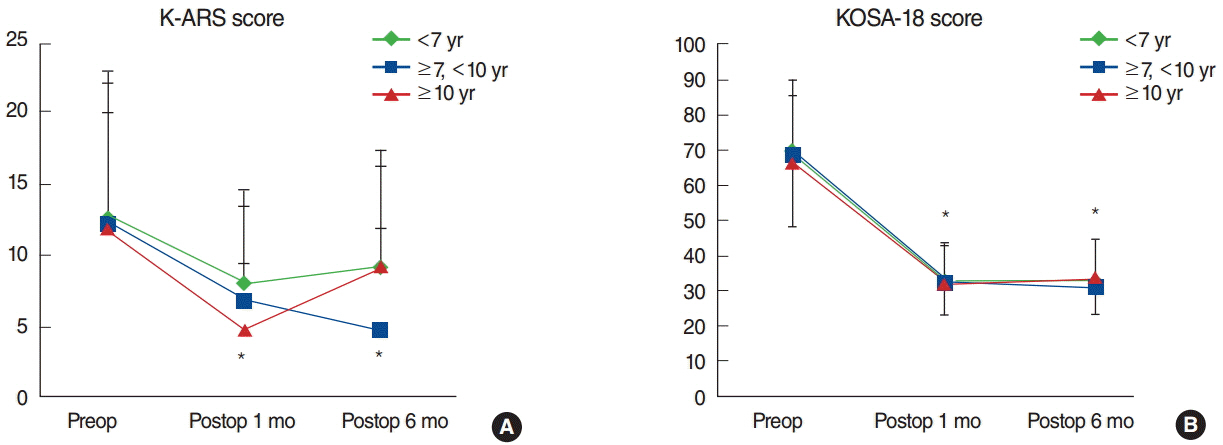
This study prospectively enrolled 148 children who underwent AT for SDB. Caregivers filled out Korean attention deficit hyperactivity disorder (ADHD) rating scale (K-ARS) and Korean version of the obstructive sleep apnea-18 (KOSA-18) at preoperative 1 day, postoperative 1 month, and postoperative 6 months. Longitudinal changes in K-ARS and KOSA-18 were evaluated and compared among subgroups.
RESULTS
Both K-ARS and KOSA-18 scores improved immediately at postoperative 1 month and were maintained at postoperative 6 months. The mean preoperative K-ARS scores of the non-ADHD, ADHD-trait, and overt-ADHD groups showed uniformly immediate and sustained improvements. Also, the mean preoperative KOSA-18 scores of the small, moderate, and large impact groups were significantly improved both at postoperative 1 month and 6 months. The changes in behavior and QoL showed no significant differences with regard to the aforementioned factors.
CONCLUSION
After AT, we may expect immediate and sustained improvements in behavior and QoL in children with SDB regardless of preoperative symptom severity. Moreover, by performing AT, improvements in behavior and QoL are expected regardless of sex, age, allergic trait, or concurrent coblation-assisted turbinoplasty. These findings may help our colleague physicians counselling pediatric SDB patients and their caregivers.
Keyword
MeSH Terms
Figure
Reference
-
1. De Serres LM, Derkay C, Sie K, Biavati M, Jones J, Tunkel D, et al. Impact of adenotonsillectomy on quality of life in children with obstructive sleep disorders. Arch Otolaryngol Head Neck Surg. 2002; May. 128(5):489–96.
Article2. Spruyt K, Gozal D. Sleep disturbances in children with attentiondeficit/hyperactivity disorder. Expert Rev Neurother. 2011; Apr. 11(4):565–77.
Article3. Huang YS, Guilleminault C, Li HY, Yang CM, Wu YY, Chen NH. Attention-deficit/hyperactivity disorder with obstructive sleep apnea: a treatment outcome study. Sleep Med. 2007; Jan. 8(1):18–30.
Article4. Bhattacharjee R, Kheirandish-Gozal L, Spruyt K, Mitchell RB, Promchiarak J, Simakajornboon N, et al. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: a multicenter retrospective study. Am J Respir Crit Care Med. 2010; Sep. 182(5):676–83.5. Wei JL, Bond J, Mayo MS, Smith HJ, Reese M, Weatherly RA. Improved behavior and sleep after adenotonsillectomy in children with sleep-disordered breathing: long-term follow-up. Arch Otolaryngol Head Neck Surg. 2009; Jul. 135(7):642–6.
Article6. Baldassari CM, Mitchell RB, Schubert C, Rudnick EF. Pediatric obstructive sleep apnea and quality of life: a meta-analysis. Otolaryngol Head Neck Surg. 2008; Mar. 138(3):265–73.
Article7. Mitchell RB, Kelly J. Long-term changes in behavior after adenotonsillectomy for obstructive sleep apnea syndrome in children. Otolaryngol Head Neck Surg. 2006; Mar. 134(3):374–8.
Article8. McColley SA, Carroll JL, Curtis S, Loughlin GM, Sampson HA. High prevalence of allergic sensitization in children with habitual snoring and obstructive sleep apnea. Chest. 1997; Jan. 111(1):170–3.
Article9. Yoo HJ, Cho SC, Ha J, Yune SK, Kim SJ, Hwang J, et al. Attention deficit hyperactivity symptoms and internet addiction. Psychiatry Clin Neurosci. 2004; Oct. 58(5):487–94.
Article10. DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD rating scaleIV: checklists, norms, and clinical interpretation. New York: Guilford Press;1998.11. Katic A, Dirks B, Babcock T, Scheckner B, Adeyi B, Richards C, et al. Treatment outcomes with lisdexamfetamine dimesylate in children who have attention-deficit/hyperactivity disorder with emotional control impairments. J Child Adolesc Psychopharmacol. 2013; Aug. 23(6):386–93.
Article12. Hwang SH, Guilleminault C, Park CS, Kim TW, Hong SC. Usefulness of adenotonsillar size for prediction of severity of obstructive sleep apnea and flow limitation. Otolaryngol Head Neck Surg. 2013; Aug. 149(2):326–34.
Article13. Fischer Y, Rettinger G, Dorn M. Long term change in quality of life after adenotonsillectomy for pediatric obstructive sleep disorders. Laryngorhinootologie. 2006; Nov. 85(11):809–18.14. Franco RA Jr, Rosenfeld RM, Rao M. First place: resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000; Jul. 123(1 Pt 1):9–16.15. Mitchell RB, Kelly J. Child behavior after adenotonsillectomy for obstructive sleep apnea syndrome. Laryngoscope. 2005; Nov. 115(11):2051–5.
Article16. Li HY, Huang YS, Chen NH, Fang TJ, Lee LA. Impact of adenotonsillectomy on behavior in children with sleep-disordered breathing. Laryngoscope. 2006; Jul. 116(7):1142–7.
Article17. Friedman BC, Hendeles-Amitai A, Kozminsky E, Leiberman A, Friger M, Tarasiuk A, et al. Adenotonsillectomy improves neurocognitive function in children with obstructive sleep apnea syndrome. Sleep. 2003; Dec. 26(8):999–1005.
Article18. Dillon JE, Blunden S, Ruzicka DL, Guire KE, Champine D, Weatherly RA, et al. DSM-IV diagnoses and obstructive sleep apnea in children before and 1 year after adenotonsillectomy. J Am Acad Child Adolesc Psychiatry. 2007; Nov. 46(11):1425–36.
Article19. Strocker AM, Shapiro NL. Parental understanding and attitudes of pediatric obstructive sleep apnea and adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2007; Nov. 71(11):1709–15.
Article20. Cheng PW, Fang KM, Su HW, Huang TW. Improved objective outcomes and quality of life after adenotonsillectomy with inferior turbinate reduction in pediatric obstructive sleep apnea with inferior turbinate hypertrophy. Laryngoscope. 2012; Dec. 122(12):2850–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Quality of Life after Adenotonsillectomy in Children with Sleep Disordered Breathing
- Effect of Adenotonsillectomy on Inattention and Hyperactivity in Children with Sleep Disordered Breathing
- Changes of Sleep Disordered Breathing and Quality of Life after Adenotonsillectomy in Pediatric Obstructive Sleep Apnea
- Allergic Rhinitis and Sleep-disordered Breathing
- Nasopharyngeal Width and Its Association With Sleep-Disordered Breathing Symptoms in Children