Clin Endosc.
2016 May;49(3):298-302. 10.5946/ce.2015.114.
Hybrid Natural Orifice Transluminal Endoscopic Surgery with Sentinel Lymph Node Navigation for Deep Early Gastric Cancer in the Fundic Region
- Affiliations
-
- 1Department of Internal Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea. shkim@eulji.ac.kr
- 2Department of Surgery, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
- KMID: 2165026
- DOI: http://doi.org/10.5946/ce.2015.114
Abstract
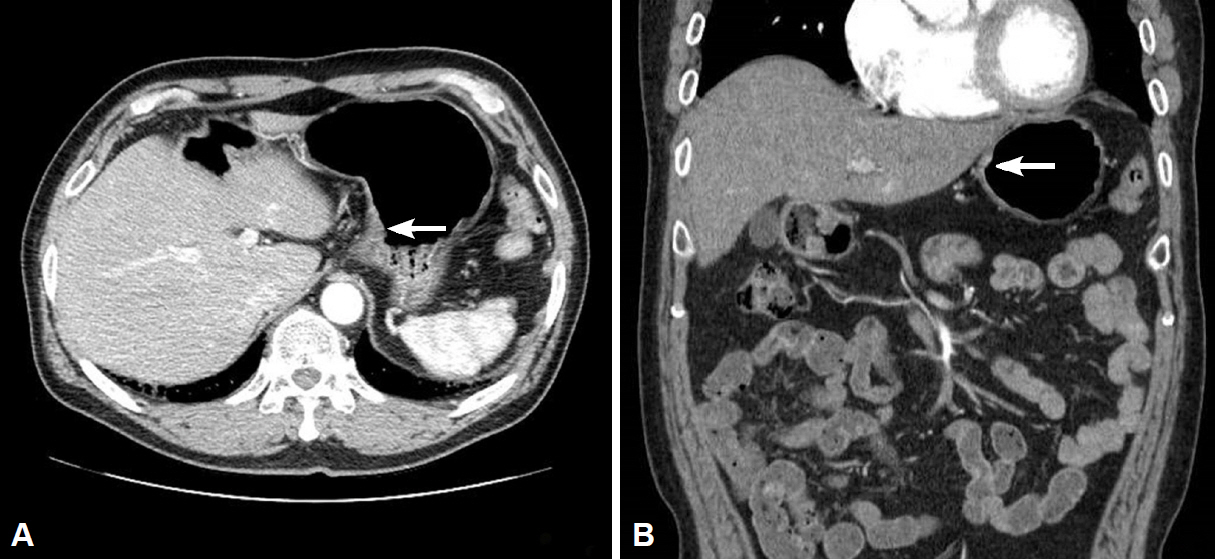
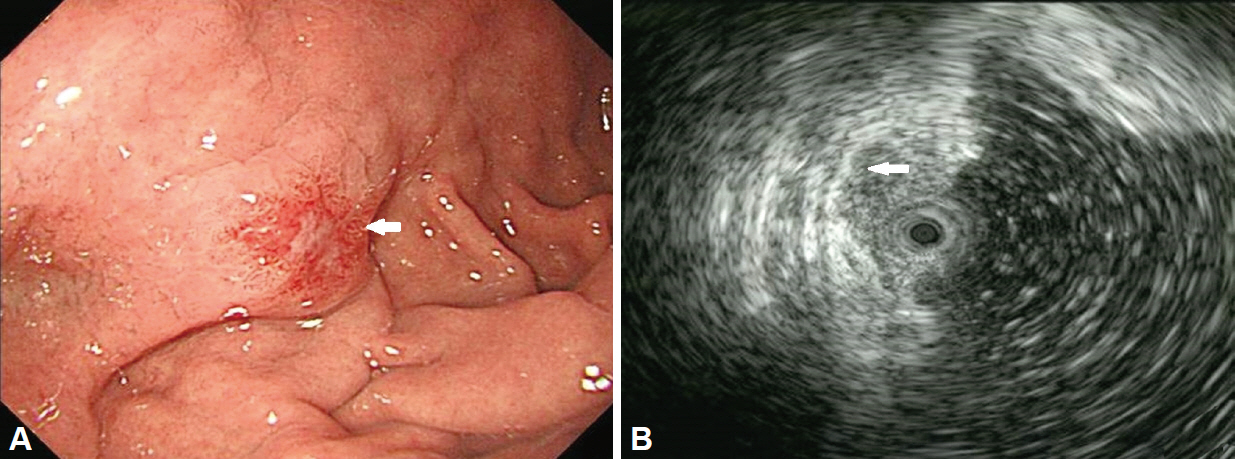
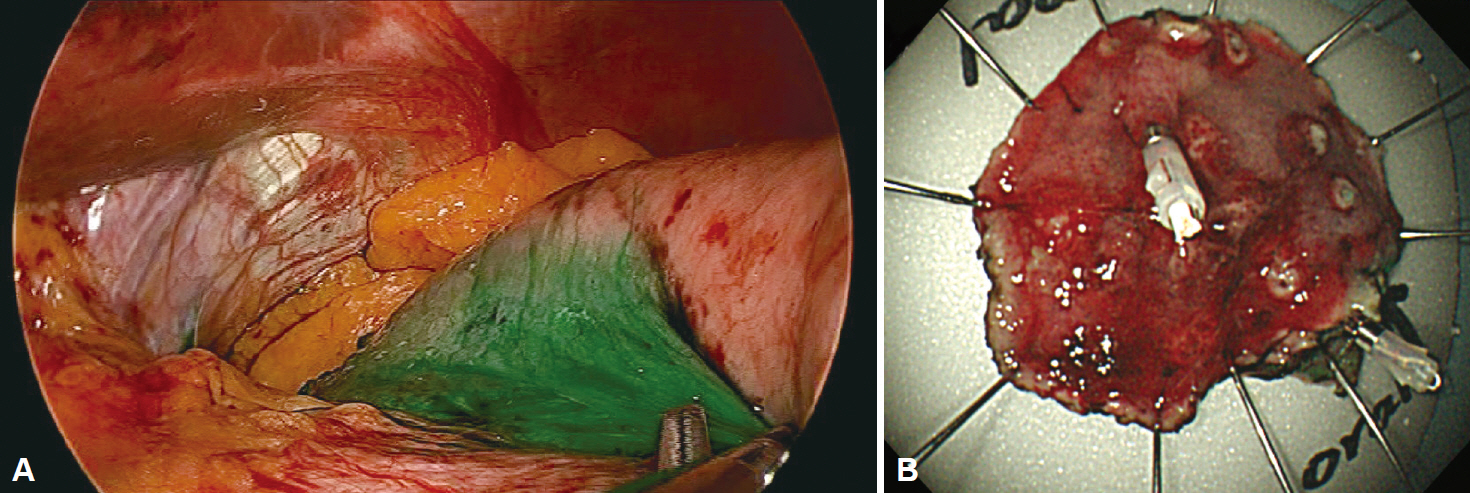
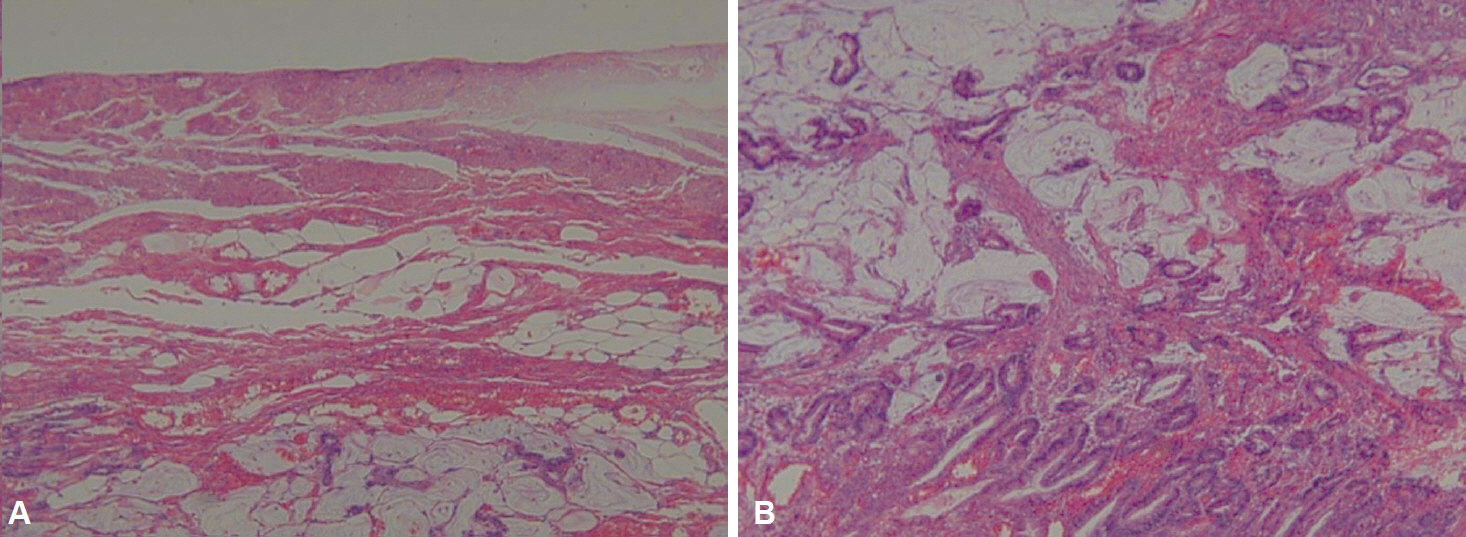
- For patients refusing surgical treatment for deep early gastric cancer, hybrid natural orifice transluminal endoscopic surgery with sentinel lymph node navigation is a potential treatment option, particularly when the anatomic location of the cancer has low probability of lymph node metastasis. We report a case of deep early gastric cancer of the fundus beyond the endoscopic submucosal dissection indication that was treated by hybrid natural orifice transluminal endoscopic surgery with sentinel lymph node navigation. In a conventional approach, a total gastrectomy would have been needed; however, the patient refused surgical intervention. In this case, since the patient showed no positivity of the sentinel lymph node on intraoperative navigation, laparoscopic basin lymph node dissection was not performed. Hybrid natural orifice transluminal endoscopic surgery might be considered for specific regions such as the safety zone where lymph node metastases are less likely to occur.
MeSH Terms
Figure
Cited by 1 articles
-
Current Status of Endoscopic Resection of Early Gastric Cancer in Korea
Hwoon-Yong Jung
Korean J Gastroenterol. 2017;70(3):121-127. doi: 10.4166/kjg.2017.70.3.121.
Reference
-
1. Isozaki H, Okajima K, Yamada S, et al. Proximal subtotal gastrectomy for the treatment of carcinoma of the upper third of the stomach: its indications based on lymph node metastasis and perigastric lymphatic flow. Surg Today. 1995; 25:21–26.
Article2. Li H, Lu P, Lu Y, et al. Predictive factors for lymph node metastasis in poorly differentiated early gastric cancer and their impact on the surgical strategy. World J Gastroenterol. 2008; 14:4222–4226.
Article3. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225.
Article4. Hirasawa T, Gotoda T, Miyata S, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009; 12:148–152.
Article5. Kwee RM, Kwee TC. Predicting lymph node status in early gastric cancer. Gastric Cancer. 2008; 11:134–148.
Article6. Cho WY, Kim YJ, Cho JY, et al. Hybrid natural orifice transluminal endoscopic surgery: endoscopic full-thickness resection of early gastric cancer and laparoscopic regional lymph node dissection: 14 human cases. Endoscopy. 2011; 43:134–139.7. Draşovean R. Post-gastrectomy syndromes. Acta Medica Transilv. 2012; 2:201–203.8. Ren G, Cai R, Zhang WJ, Ou JM, Jin YN, Li WH. Prediction of risk factors for lymph node metastasis in early gastric cancer. World J Gastroenterol. 2013; 19:3096–3107.
Article9. Boku T, Nakane Y, Okusa T, et al. Strategy for lymphadenectomy of gastric cancer. Surgery. 1989; 105:585–592.10. Kitamura M, Arai K, Miyashita K. Indication and clinical results of proximal gastrectomy with special reference to lymph node metastasis in upper gastric cancers. J Jpn Pract Surg Soc. 1991; 52:1454–1460.
Article11. Symeonidis D, Koukoulis G, Tepetes K. Sentinel node navigation surgery in gastric cancer: current status. World J Gastrointest Surg. 2014; 6:88–93.
Article12. Tajima Y, Murakami M, Yamazaki K, et al. Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol. 2010; 17:1787–1793.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Natural Orifice Transluminal Endoscopic Surgery and Upper Gastrointestinal Tract
- The current status and future perspectives of laparoscopic surgery for gastric cancer
- Recent development of innovative resection methods for gastric neoplasms using hybrid natural orifice transluminal endoscopic surgery approach
- Recent Advances in Sentinel Node Navigation Surgery for Early Gastric Cancer
- Endoscopic Resection of Early Gastric Cancer