Clin Endosc.
2016 May;49(3):229-231. 10.5946/ce.2016.035.
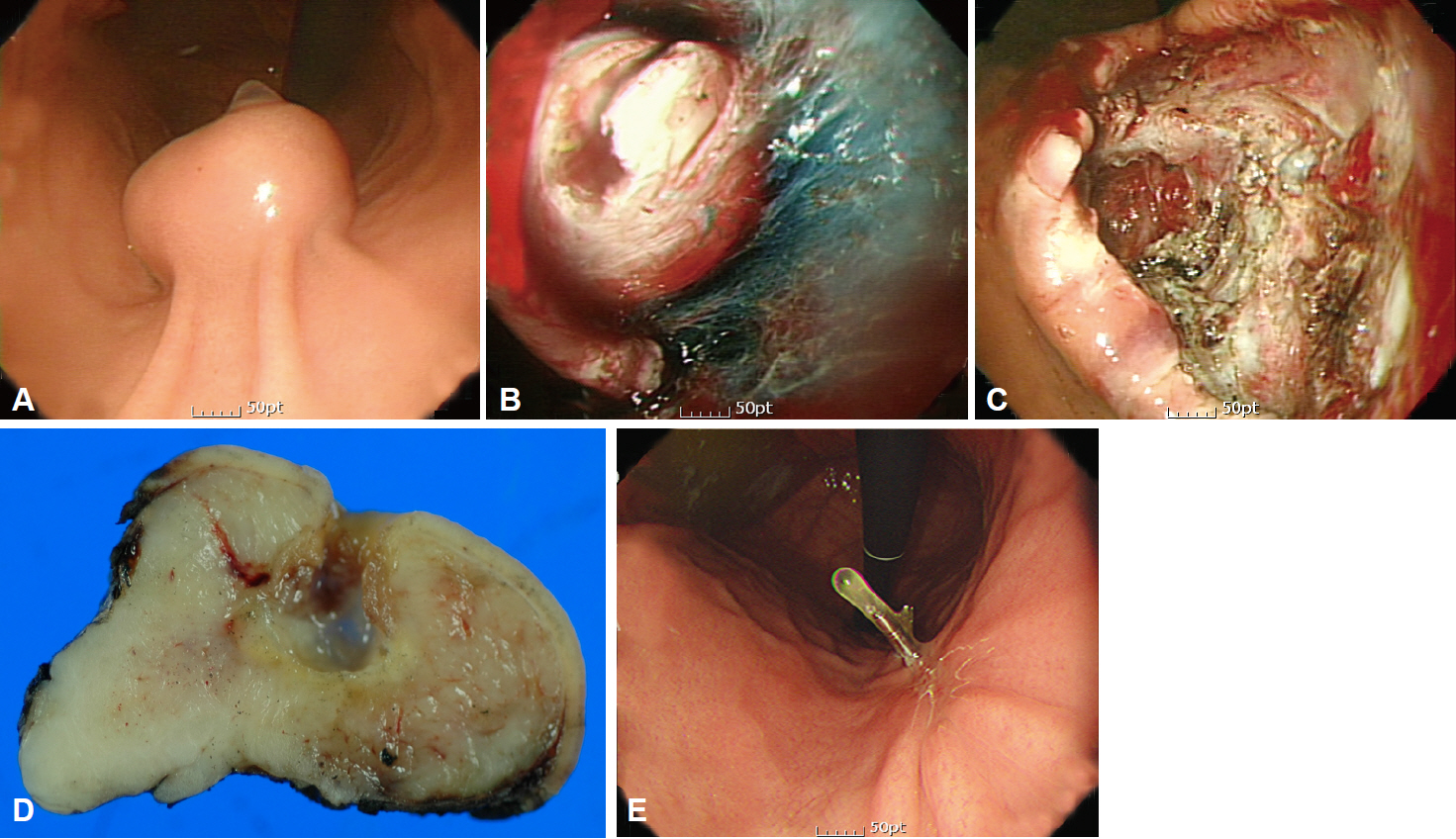
Interpretation of Pathologic Margin after Endoscopic Resection of Gastrointestinal Stromal Tumor
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea. harley@snu.ac.kr
- KMID: 2165016
- DOI: http://doi.org/10.5946/ce.2016.035
Abstract
- Interpretation of the pathologic margin of a specimen from a resected tumor is important because local recurrence can be predicted by the presence of tumor cells in the resection margin. Although a sufficient resection margin is recommended in the resection of gastrointestinal adenocarcinoma, it is not usually regarded strictly in cases of mesenchymal tumor, especially gastrointestinal stromal tumor (GIST), because the tumor is usually encapsulated or well demarcated, and not infiltrative. Therefore, margin positivity is not rare in the pathological evaluation of surgically or endoscopically resected GIST, and does not always indicate incomplete resection. Although a GIST may have a tumor-positive pathologic margin, complete resection may be achieved if no residual tumor is visible, and long-term survival can be predicted as in the cases with a negative pathologic margin.
Figure
Reference
-
1. Gouveia AM, Pimenta AP, Capelinha AF, de la Cruz D, Silva P, Lopes JM. Surgical margin status and prognosis of gastrointestinal stromal tumor. World J Surg. 2008; 32:2375–2382.
Article2. Ng EH, Pollock RE, Munsell MF, Atkinson EN, Romsdahl MM. Prognostic factors influencing survival in gastrointestinal leiomyosarcomas. Implications for surgical management and staging. Ann Surg. 1992; 215:68–77.
Article3. Dematteo RP, Heinrich MC, El-Rifai WM, Demetri G. Clinical management of gastrointestinal stromal tumors: before and after STI-571. Hum Pathol. 2002; 33:466–477.
Article4. Kim MY, Park YS, Choi KD, et al. Predictors of recurrence after resection of small gastric gastrointestinal stromal tumors of 5 cm or less. J Clin Gastroenterol. 2012; 46:130–137.
Article5. McCarter MD, Antonescu CR, Ballman KV, et al. Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg. 2012; 215:53–59.
Article6. Joo MK, Park JJ, Kim H, et al. Endoscopic versus surgical resection of GI stromal tumors in the upper GI tract. Gastrointest Endosc. 2016; 83:318–326.
Article7. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000; 231:51–58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Outcomes after Endoscopic Treatment of Gastric Gastrointestinal Stromal Tumor
- Endoscopic Resection of Gastrointestinal Stromal Tumor: Is It Safe?
- Malignant Transformation of Gastric Gastrointestinal Stromal Tumor in 44 Months Observational Period: A Case Report
- Evaluation and Endoscopic Management of Esophageal Submucosal Tumor
- Current Techniques for Treating Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract