Yonsei Med J.
2015 Sep;56(5):1443-1448. 10.3349/ymj.2015.56.5.1443.
Snakebite in Korea: A Guideline to Primary Surgical Management
- Affiliations
-
- 1Department of Orthopedics, Yonsei University Wonju College of Medicine, Wonju, Korea. nakjh78@naver.com
- 2Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Emergency Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2163642
- DOI: http://doi.org/10.3349/ymj.2015.56.5.1443
Abstract
- PURPOSE
Snakebite is an emergency which causes local symptoms such as pain and edema around the bite. Systemic symptoms may also develop, such as dizziness or renal failure, and may even cause death. The purpose of this research was to assess the validity and safety of snakebite protocol for surgery when treating snakebite patients.
MATERIALS AND METHODS
Retrospective research was performed on patients who were admitted after being treated at the emergency center from January 2008 to December 2012. When necessary, debridement was also performed, and 46 of 111 patients (41.4%) underwent debridement. Those who had received debridement without antivenom administration due to a positive skin reaction test were classified as group A, and group B received antivenom and delayed debridement. We reviewed the emergency and admission charts of the patients in each group and recorded and compared their age, sex, bite site, severity of local and general symptoms, time to receive antivenin, and complications.
RESULTS
Of the ten patients (21.7%) in group A, two (66.6%) developed cellulites, and one of them experienced skin necrosis, resulting in a skin graft. In group B, there were 36 patients (78.2%), 19 (52.7%) of whom developed cellulitis. Skin necrosis occurred in two patients, and one of these patients received a skin graft. Compartment syndrome was found in one patient, and fasciotomy and a skin graft were performed.
CONCLUSION
The treatment protocol implemented to treat snakebite patients admitted to the emergency center during this research was safely and properly followed during surgical treatment.
Keyword
MeSH Terms
-
Adult
Aged
Antivenins/administration & dosage
Combined Modality Therapy
Compartment Syndromes
Debridement/*methods
Disease Management
Edema/etiology
Female
Humans
Male
Middle Aged
Necrosis
*Practice Guidelines as Topic
Republic of Korea
Retrospective Studies
Severity of Illness Index
Skin/pathology
Skin Transplantation/*methods
Snake Bites/complications/*diagnosis/pathology/*surgery
Snake Venoms/adverse effects
Soft Tissue Injuries/etiology/*pathology/surgery
Treatment Outcome
Wound Healing/physiology
Antivenins
Snake Venoms
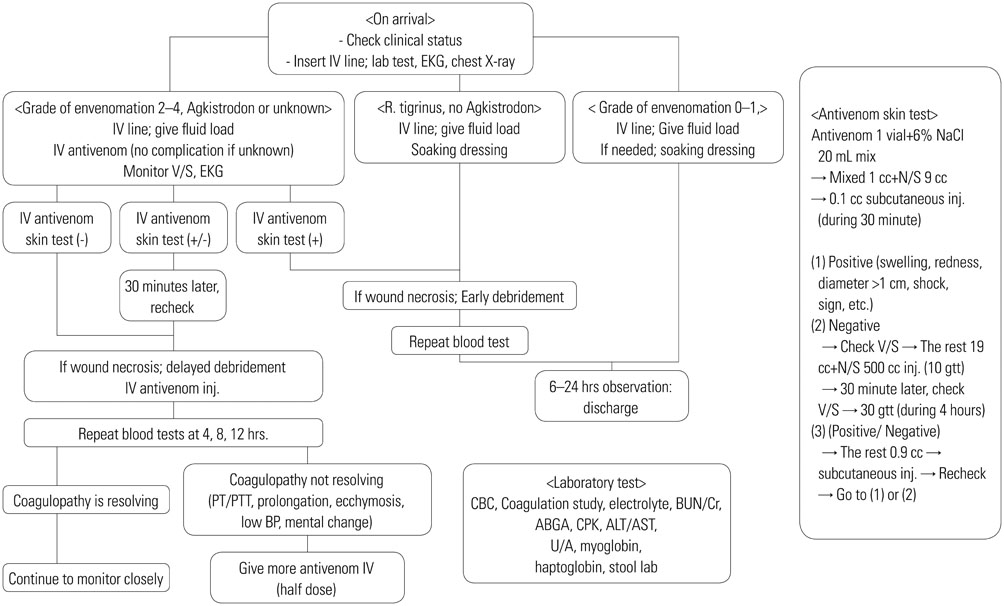
Figure
Cited by 1 articles
-
Case of Treatment of Snakebite on Finger with Topical Oxygen Therapy
Hwan Jun Choi, Da Woon Lee, Hyeong Rae Ryu, Jun Hyuk Kim, Jun Ho Lee
Arch Hand Microsurg. 2020;25(4):292-296. doi: 10.12790/ahm.20.0061.
Reference
-
1. Parrish HM. Incidence of treated snakebites in the United States. Public Health Rep. 1966; 81:269–276.2. Warrell DA. Venomous bites and stings in the tropical world. Med J Aust. 1993; 159:773–779.3. Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F. Snake bite in South Asia: a review. PLoS Negl Trop Dis. 2010; 4:e603.
Article4. Jang IS, Lee JA, Kim SY, Hyun SC, Park SM, Park JS, et al. Clinical features in snake bite. J Korean Soc Emerg Med. 1996; 7:580–589.5. Shin CS, Bae JS, Sohn KS. Clinical Analysis on Venomous Snake Bite in Korea. J Korean Surg Soc. 1984; 27:245–254.6. Toschlog EA, Bauer CR, Hall EL, Dart RC, Khatri V, Lavonas EJ. Surgical considerations in the management of pit viper snake envenomation. J Am Coll Surg. 2013; 217:726–735.
Article7. Lee BJ, Hong SI, Kim HS, Kim TH, Lee JH, Kim HJ, et al. Hematological features of coagulopathy and the efficacy of antivenin therapy for a Korean snakebite. J Korean Surg Soc. 2007; 72:18–26.8. Shim JH, Son YJ, Lee SS, Park KS, Oh HB, Park YD. Ecological study on poisonous snake and investigation of the venom characteristics, snakebiting frequency in Korea. Korean J Env Eco. 1998; 12:58–77.9. Oh SJ, Yoo IH, Kim JP. A clinical review of venomous snake bite. J Korean Surg Soc. 1982; 24:1236–1244.10. Kim ES, Choi WJ. Clinical review of venomous snake bite. J Korean Surg Soc. 2000; 59:433–440.11. Russell FE. Snake venom poisoning in the United States. Annu Rev Med. 1980; 31:247–259.
Article12. Glass TG Jr. Early debridement in pit viper bite. Surg Gynecol Obstet. 1973; 136:774–776.13. Huang TT, Lynch JB, Larson DL, Lewis SR. The use of excisional therapy in the management of snakebite. Ann Surg. 1974; 179:598–607.
Article14. Glass TG Jr. Early debridement in pit viper bites. JAMA. 1976; 235:2513–2516.
Article15. Glass TG Jr. Treatment of rattlesnake bites. JAMA. 1982; 247:461.
Article16. Huang TT, Blackwell SJ, Lewis SR. Hand deformities in patients with snakebite. Plast Reconstr Surg. 1978; 62:32–36.
Article17. Huang TT, Blackwell SJ, Lewis SR. Tissue necrosis in snakebite. Tex Med. 1981; 77:53–58.18. Cohen WR, Wetzel W, Kadish A. Local heat and cold application after eastern cottonmouth moccasin (Agkistrodon piscivorus) envenomation in the rat: effect on tissue injury. Toxicon. 1992; 30:1383–1386.
Article19. Frank HA. Snakebite or frostbite: what are we doing? An evaluation of cryotherapy for envenomation. Calif Med. 1971; 114:25–27.20. Lavonas EJ, Kokko J, Schaeffer TH, Mlynarchek SL, Bogdan GM, Dart RC. Short-term outcomes after Fab antivenom therapy for severe crotaline snakebite. Ann Emerg Med. 2011; 57:128–137.
Article21. Dart RC, Seifert SA, Boyer LV, Clark RF, Hall E, McKinney P, et al. A randomized multicenter trial of crotalinae polyvalent immune Fab (ovine) antivenom for the treatment for crotaline snakebite in the United States. Arch Intern Med. 2001; 161:2030–2036.
Article22. Yin S, Kokko J, Lavonas E, Mlynarchek S, Bogdan G, Schaeffer T. Factors associated with difficulty achieving initial control with crotalidae polyvalent immune fab antivenom in snakebite patients. Acad Emerg Med. 2011; 18:46–52.
Article23. Dart RC, Seifert SA, Carroll L, Clark RF, Hall E, Boyer-Hassen LV, et al. Affinity-purified, mixed monospecific crotalid antivenom ovine Fab for the treatment of crotalid venom poisoning. Ann Emerg Med. 1997; 30:33–39.
Article24. Lavonas EJ, Gerardo CJ, O'Malley G, Arnold TC, Bush SP, Banner W Jr, et al. Initial experience with Crotalidae polyvalent immune Fab (ovine) antivenom in the treatment of copperhead snakebite. Ann Emerg Med. 2004; 43:200–206.
Article25. Ruha AM, Curry SC, Beuhler M, Katz K, Brooks DE, Graeme KA, et al. Initial postmarketing experience with crotalidae polyvalent immune Fab for treatment of rattlesnake envenomation. Ann Emerg Med. 2002; 39:609–615.
Article26. Ruha AM, Curry SC, Albrecht C, Riley B, Pizon A. Late hematologic toxicity following treatment of rattlesnake envenomation with crotalidae polyvalent immune Fab antivenom. Toxicon. 2011; 57:53–59.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum to "Snakebite in Korea: A Guideline to Primary Surgical Management" by Rha JH, et al. (Yonsei Med J 2015;56:1443-8.)
- 2014 KLCSG-NCC Korea Practice Guideline for the Management of Hepatocellular Carcinoma
- Unilateral Vestibular Neuritis after Snakebite: Is There a Causal Relationship?
- Coagulopathy in patients who experience snakebite
- Fasciotomy in compartment syndrome from snakebite