Yonsei Med J.
2015 Sep;56(5):1389-1394. 10.3349/ymj.2015.56.5.1389.
Development of Thyroid-Associated Ophthalmopathy in Patients Who Underwent Total Thyroidectomy
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 2Department of Medicine, Yonsei University Graduate School of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Konyang University College of Medicine, Daejeon, Korea.
- 4Division of Endocrinology & Metabolism, Department of Internal Medicine, Soonchunhyang Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 5Department of Ophthalmology, Severance Hospital, Institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea. yoonjs@yuhs.ac
- KMID: 2163634
- DOI: http://doi.org/10.3349/ymj.2015.56.5.1389
Abstract
- PURPOSE
To report clinical characteristics of thyroid-associated ophthalmopathy (TAO) in patients who previously underwent total thyroidectomy for thyroid cancer or a benign mass of the thyroid.
MATERIALS AND METHODS
Of the patients who were diagnosed with TAO from March 2008 to March 2012, we performed a retrospective chart review on those who had undergone total thyroidectomy for thyroid cancer or a benign mass of the thyroid before the occurrence of ophthalmopathy.
RESULTS
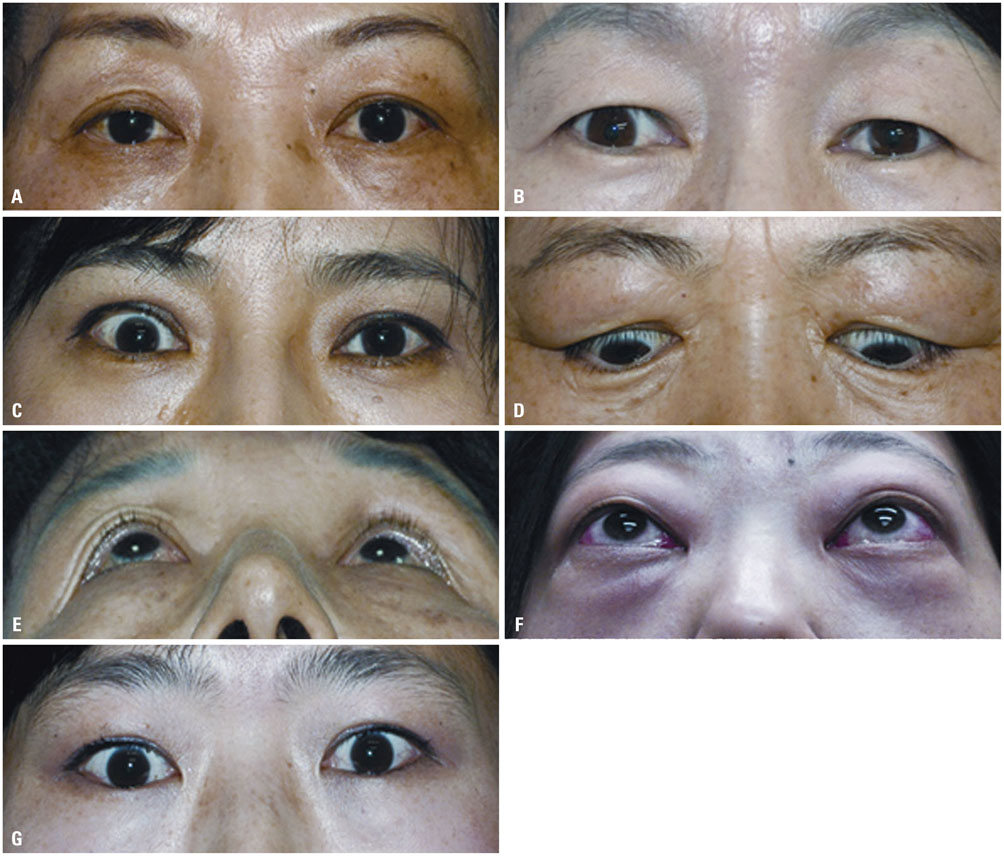
Of the 206 patients diagnosed with TAO, seven (3.4%) met the inclusion criteria. The mean age of the subjects was 47.4 years, and all were female. Six patients were diagnosed with papillary thyroid cancer, and one was diagnosed with a benign mass. The duration between total thyroidectomy and onset of TAO ranged from 3-120 months (median 48 months). Ophthalmic manifestations varied among cases. Except for the patient who was diagnosed with a benign mass, all patients showed hyperthyroid status and were under Synthroid hormone treatment at the time of TAO development. Five of these six patients had positive levels of thyroid-stimulating hormone (TSH) receptor autoantibodies.
CONCLUSION
TAO rarely develops after total thyroidectomy, and the mechanism of TAO occurrence is unclear. However, most patients showed abnormalities in thyroid function and TSH receptor autoantibodies.
Keyword
MeSH Terms
-
Adult
Aged
Autoantibodies/blood
Carcinoma
Carcinoma, Papillary/immunology/surgery
Female
Graves Ophthalmopathy/*diagnosis/immunology
Humans
Male
Middle Aged
Postoperative Complications/etiology/immunology/pathology
Receptors, Thyrotropin
Retrospective Studies
Thyroid Neoplasms/complications/*surgery
Thyroidectomy/adverse effects/*methods
Thyrotropin/blood
Treatment Outcome
Autoantibodies
Receptors, Thyrotropin
Thyrotropin
Figure
Reference
-
1. Bahn RS. Graves' ophthalmopathy. N Engl J Med. 2010; 362:726–738.
Article2. Kuriyan AE, Phipps RP, Feldon SE. The eye and thyroid disease. Curr Opin Ophthalmol. 2008; 19:499–506.
Article3. Antonelli A, Ferrari SM, Corrado A, Franceschini SS, Gelmini S, Ferrannini E, et al. Extra-ocular muscle cells from patients with Graves' ophthalmopathy secrete α (CXCL10) and β (CCL2) chemokines under the influence of cytokines that are modulated by PPARγ. Autoimmun Rev. 2014; 13:1160–1166.
Article4. Antonelli A, Ferrari SM, Giuggioli D, Ferrannini E, Ferri C, Fallahi P. Chemokine (C-X-C motif) ligand (CXCL)10 in autoimmune diseases. Autoimmun Rev. 2014; 13:272–280.
Article5. Tanda ML, Piantanida E, Liparulo L, Veronesi G, Lai A, Sassi L, et al. Prevalence and natural history of Graves' orbitopathy in a large series of patients with newly diagnosed graves' hyperthyroidism seen at a single center. J Clin Endocrinol Metab. 2013; 98:1443–1449.
Article6. Lehmann GM, Feldon SE, Smith TJ, Phipps RP. Immune mechanisms in thyroid eye disease. Thyroid. 2008; 18:959–965.
Article7. Jang SY, Shin DY, Lee EJ, Yoon JS. Clinical characteristics of Graves' orbitopathy in patients showing discrepancy between levels from TBII assays and TSI bioassay. Clin Endocrinol (Oxf). 2014; 80:591–597.
Article8. Jang SY, Shin DY, Lee EJ, Choi YJ, Lee SY, Yoon JS. Correlation between TSH receptor antibody assays and clinical manifestations of Graves' orbitopathy. Yonsei Med J. 2013; 54:1033–1039.9. Lytton SD, Ponto KA, Kanitz M, Matheis N, Kohn LD, Kahaly GJ. A novel thyroid stimulating immunoglobulin bioassay is a functional indicator of activity and severity of Graves' orbitopathy. J Clin Endocrinol Metab. 2010; 95:2123–2131.
Article10. Carnell NE, Valente WA. Thyroid nodules in Graves' disease: classification, characterization, and response to treatment. Thyroid. 1998; 8:647–652.
Article11. Yu HM, Park SH, Lee JM, Park KS. Graves' Disease that Developed Shortly after Surgery for Thyroid Cancer. Endocrinol Metab (Seoul). 2013; 28:226–230.
Article12. Kasuga Y, Kobayashi S, Fujimori M, Shingu K, Hama Y, Ito K, et al. Development of Graves' disease after surgical treatment for thyroid nodules: report of four cases. Endocr J. 1997; 44:567–570.13. Menconi F, Marinò M, Pinchera A, Rocchi R, Mazzi B, Nardi M, et al. Effects of total thyroid ablation versus near-total thyroidectomy alone on mild to moderate Graves' orbitopathy treated with intravenous glucocorticoids. J Clin Endocrinol Metab. 2007; 92:1653–1658.
Article14. Winsa B, Rastad J, Akerström G, Johansson H, Westermark K, Karlsson FA. Retrospective evaluation of subtotal and total thyroidectomy in Graves' disease with and without endocrine ophthalmopathy. Eur J Endocrinol. 1995; 132:406–412.
Article15. Yoon JS, Lew H, Park JS, Nam KH, Lee SY. Papillary thyroid carcinoma with thyroid-associated orbitopathy in a euthyroid state. Ophthal Plast Reconstr Surg. 2007; 23:187–191.16. Eckstein AK, Lösch C, Glowacka D, Schott M, Mann K, Esser J, et al. Euthyroid and primarily hypothyroid patients develop milder and significantly more asymmetrical Graves ophthalmopathy. Br J Ophthalmol. 2009; 93:1052–1056.
Article17. Jang SY, Lee SY, Lee EJ, Yoon JS. Clinical features of thyroid-associated ophthalmopathy in clinically euthyroid Korean patients. Eye (Lond). 2012; 26:1263–1269.
Article18. Acharya SH, Avenell A, Philip S, Burr J, Bevan JS, Abraham P. Radioiodine therapy (RAI) for Graves' disease (GD) and the effect on ophthalmopathy: a systematic review. Clin Endocrinol (Oxf). 2008; 69:943–950.
Article19. Karlsson FA. Endocrine ophthalmopathy and radioiodine therapy. Acta Oncol. 2006; 45:1046–1050.
Article20. Woeber KA, Schwartz LK. Graves ophthalmopathy after radiation treatment of thyroid cancer. Endocr Pract. 2008; 14:419–421.
Article21. Berg G, Andersson T, Sjödell L, Jansson S, Nyström E. Development of severe thyroid-associated ophthalmopathy in a patient with disseminated thyroid cancer treated with recombinant human thyrotropin/radioiodine and retinoic acid. Thyroid. 2005; 15:1389–1394.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Manifestations of Thyroid-associated Ophthalmopathy Accompanied by Thyroid Cancer
- Development of Graves' Ophthalmopathy after Radioactive Iodine Ablation Using Recombinant Human Thyrotropin for Incidentally Discovered Papillary Thyroid Carcinoma
- Total Thyroidectomy for Graves' Disease
- Strabismus Surgery for Thyroid Ophthalmopathy
- The Effect of Previous Orbital Decompression on Outcome of Strabismus Surgery in Patients with Thyroid Ophthalmopathy