Pediatr Infect Vaccine.
2016 Apr;23(1):67-71. 10.14776/piv.2016.23.1.67.
A Case of Erythema Nodosum Associated with Mycoplasma pneumoniae Infection: Pathologic Findings and a Presumed Pathogenesis
- Affiliations
-
- 1Department of Pediatrics, Kyung Hee University School of Medicine, Seoul, Korea. chsh0414@khu.ac.kr
- 2Department of Pathology, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2163226
- DOI: http://doi.org/10.14776/piv.2016.23.1.67
Abstract
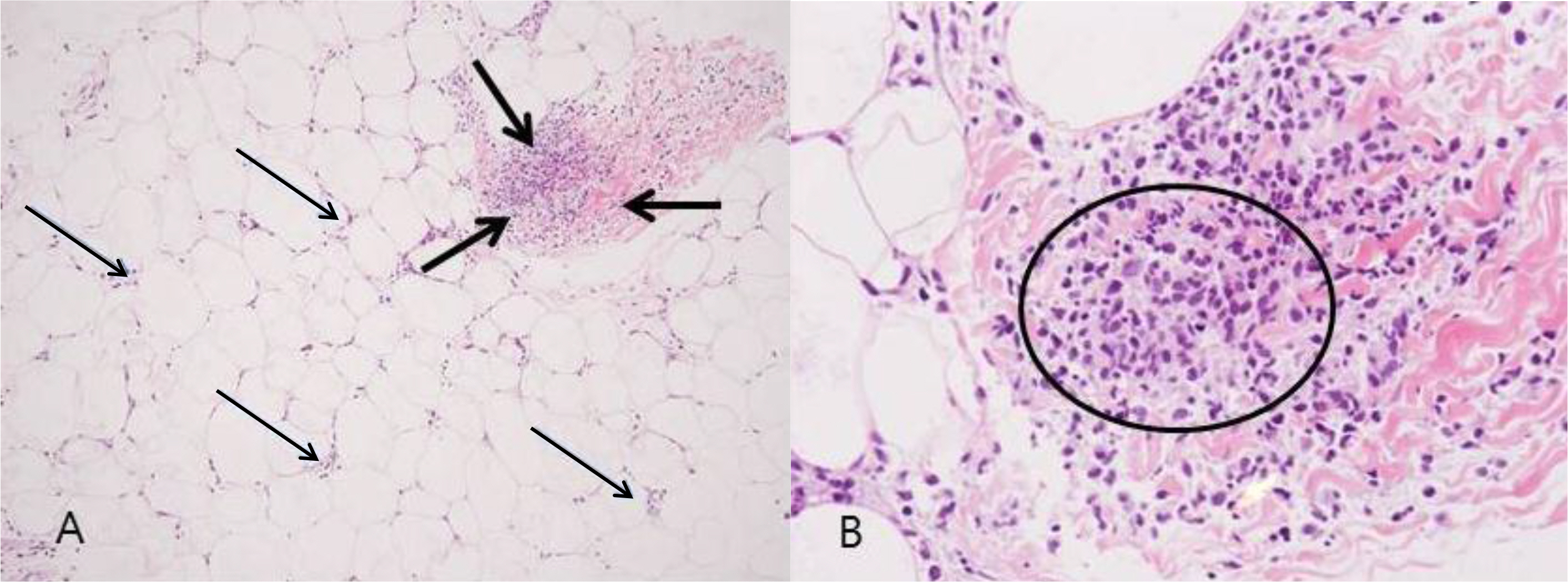
- Erythema nodosum (EN) is a painful skin disease characterized by erythematous tender nodules located predominantly over the extensor aspects of the legs. Various etiological factors, including infection, drug administration, and systemic illness have been implicated as causes of EN. Mycoplasma pneumoniae is one of rare infectious agents to cause EN in children. We report a case of a 7-year-old boy with context of respiratory illness and skin lesions with arthralgia. From stepwise approaches, IgM antibody against M. pneumoniae was positive with titers of 12.18, consistent with respiratory infection of M. pneumoniae and histopathology showed findings of septal and lobular inflammation without vasculitis consistent with EN. In addition, we reviewed the pathogenesis of this disease based on our case and the previous reports.
MeSH Terms
Figure
Reference
-
1. Polcari IC, Stein SL. Panniculitis in childhood. Dermatol Ther. 2010; 23:356–67.
Article2. Cox NH, Jorizzo IL, Bourke IF, Savage COS. Vasculitis, neutrophilic dermatoses and related disorders. Burns T, Breathnach S, Cox N, Grifliths C, editors. editors.Rook's textbook of dermatology. 8th ed.Oxford: Wiley-Blackwell;2010. p. 1282–7.
Article3. Kakourou T, Drosatou P, Psychou F, Aroni K, Nicolaidou P. Erythema nodosum in children: a prospective study. I Am Acad Dermat01. 2001; 44:17–21.
Article4. Rodriguez Blanco MA, Martin Morales IM, Casas Fernandez L. Erythematoviolaceous nodules and pneumonia. An Esp Pediatr. 2002; 57:279–80.5. Shimizu M, Hamaguchi Y, Matsushita T, Sakakibara Y, Yachie A. Sequentially appearing erythema nodosum, erythema multiforme and Henoch-Schénlein purpura in a patient With Mycoplasma pneumoniae infection: a case report. I Med Case Rep. 2012; 6:398.
Article6. Aydin-Teke T, Tanir G, Bayhan GI, Metin 0, Oz N. Erythema nodosum in children: evaluation of 39 patients. Turk] Pediatr. 2014; 56:144–9.7. Greco F, Catania R, Pira AL, Saporito M, Scalora L, Aguglia MG, et al. Erythema nodosum and Mycoplasma pneumoniae infections in childhood: Further observations in two patients and a literature review. I Clin Med Res. 2015. 72274–7.
Article8. Blake T, Manahan M, Robins K. Erythema nodosum-a review of an uncommon panniculitis. Dermatology Online Journal. 2014; 20:22376.9. Sanchez-Vargas FM, Gomez-Duarte OG. Mycoplasma pneumoniae-an emerging extra-pulmonary pathogen. Clin Microbiol Infect. 2008; 14:105- 17.10. Schalock PC, Dinulos JG. Mycoplasma pneumoniae-induced cutaneous disease. Int I Dermatol. 2009; 48:673–80.
Article11. Narita M. Pathogenesis of extrapulmonary manifestations of Mycoplasma pneumoniae infection with special reference to pneumonia. J Infect Chemother. 2010; 16:162–9.
Article12. Kano Y, Mitsuyama Y, Hirahara K, Shiohara T. Mycoplasma pneumoniae -infectioninduced erythema nodosum, ana-phylactoid purpura, and acute urticaria in 3 people in a single family. I Am Acad Dermatol. 2007; 57:33–5.
Article13. Lee KY. A common immunopathogenesis mechanism for infectious diseases: the protein-homeostasis-system hypo-thesis. Infect Chemother. 2015; 47:12–26.
Article14. Schwartz RA, Nervi S]. Erythema nodosum: a sign of systemic disease. Am Fam Physician. 2007; 75:695–700.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Erythema Multiforme in Adults Associated with Mycoplasma pneumoniae Infection
- Bullous Erythema Multiforme and Stevens-Johnson Syndrome Caused by Mycoplasma pneumoniae Infection
- Association of Mycoplasma pneumoniae in Asthma Pathogenesis
- The clinical and histopatholgical study of erythema induratum and erythema nodosum
- A Case of Cerebral Infarction Complicated by Mycoplasma pneumoniae Pneumonia