Diabetes Metab J.
2016 Apr;40(2):140-146. 10.4093/dmj.2016.40.2.140.
Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. janghak@snu.ac.kr
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 3Department of Orthopaedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea.
- 4Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 5Department of Neuropsychiatry, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2162085
- DOI: http://doi.org/10.4093/dmj.2016.40.2.140
Abstract
- BACKGROUND
The study aimed to investigate the influence of hyperglycemia on muscle quality in older men with type 2 diabetes.
METHODS
This was a subsidiary study of the Korean Longitudinal Study of Health and Aging. Among 326 older men consenting to tests of body composition and muscle strength, 269 men were ultimately analyzed after the exclusion because of stroke (n=30) and uncertainty about the diagnosis of diabetes (n=27). Body composition was measured using dual-energy X-ray absorptiometry and computed tomography. Muscle strength for knee extension was measured using an isokinetic dynamometer. Muscle quality was assessed from the ratio of leg strength to the entire corresponding leg muscle mass.
RESULTS
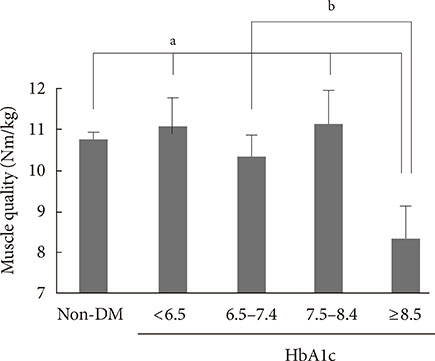
The muscle mass, strength, and quality in patients with type 2 diabetes did not differ significantly from controls. However, when patients with diabetes were subdivided according to their glycemic control status, patients with a glycosylated hemoglobin (HbA1c) level of ≥8.5% showed significantly decreased leg muscle quality by multivariate analysis (odds ratio, 4.510; P=0.045) after adjustment for age, body mass index, smoking amount, alcohol consumption, physical activity, and duration of diabetes. Physical performance status was also impaired in subjects with an HbA1c of ≥8.5%.
CONCLUSION
Poor glycemic control in these older patients with diabetes was associated with significant risk of decreased muscle quality and performance status. Glycemic control with an HbA1c of <8.5% might be needed to reduce the risk of adverse skeletal and functional outcomes in this population.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Management of Elderly Diabetes Patients Who Are Unable to Self-Care
Bok Rye Song
J Korean Diabetes. 2018;19(4):232-236. doi: 10.4093/jkd.2018.19.4.232.Diabetes and Sarcopenia
Dong Hyun Kim, Tae Yang Yu
J Korean Diabetes. 2017;18(4):239-247. doi: 10.4093/jkd.2017.18.4.239.
Reference
-
1. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M. European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–423.2. Abellan van Kan G. Epidemiology and consequences of sarcopenia. J Nutr Health Aging. 2009; 13:708–712.3. Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997; 45:92–100.4. Kim JH, Lim S, Choi SH, Kim KM, Yoon JW, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci. 2014; 69:1244–1252.5. De Rekeneire N, Resnick HE, Schwartz AV, Shorr RI, Kuller LH, Simonsick EM, Vellas B, Harris TB. Health, Aging, and Body Composition study. Diabetes is associated with subclinical functional limitation in nondisabled older individuals: the health, aging, and body composition study. Diabetes Care. 2003; 26:3257–3263.6. Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Diabetes Care. 2010; 33:1055–1060.7. Ahroni JH, Boyko EJ, Davignon DR, Pecoraro RE. The health and functional status of veterans with diabetes. Diabetes Care. 1994; 17:318–321.8. Caruso LB, Silliman RA, Demissie S, Greenfield S, Wagner EH. What can we do to improve physical function in older persons with type 2 diabetes? J Gerontol A Biol Sci Med Sci. 2000; 55:M372–M377.9. Kim JH, Choi SH, Lim S, Yoon JW, Kang SM, Kim KW, Lim JY, Cho NH, Jang HC. Sarcopenia and obesity: gender-different relationship with functional limitation in older persons. J Korean Med Sci. 2013; 28:1041–1047.10. Lim S, Yoon JW, Choi SH, Park YJ, Lee JJ, Park JH, Lee SB, Kim KW, Lim JY, Kim YB, Park KS, Lee HK, Cho SI, Jang HC. Combined impact of adiponectin and retinol-binding protein 4 on metabolic syndrome in elderly people: the Korean Longitudinal Study on Health and Aging. Obesity (Silver Spring). 2010; 18:826–832.11. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010; Suppl 1. S62–S69.12. Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999; 52:643–651.13. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994; 49:M85–M94.14. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995; 332:556–561.15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.16. Park SW, Goodpaster BH, Strotmeyer ES, de Rekeneire N, Harris TB, Schwartz AV, Tylavsky FA, Newman AB. Decreased muscle strength and quality in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes. 2006; 55:1813–1818.17. Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol (1985). 2003; 95:1717–1727.18. Jones TE, Stephenson KW, King JG, Knight KR, Marshall TL, Scott WB. Sarcopenia: mechanisms and treatments. J Geriatr Phys Ther. 2009; 32:83–89.19. Scheck SH, Barnard RJ, Lawani LO, Youngren JF, Martin DA, Singh R. Effects of NIDDM on the glucose transport system in human skeletal muscle. Diabetes Res. 1991; 16:111–119.20. Taaffe DR, Harris TB, Ferrucci L, Rowe J, Seeman TE. Cross-sectional and prospective relationships of interleukin-6 and C-reactive protein with physical performance in elderly persons: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci. 2000; 55:M709–M715.21. Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002; 57:M326–M332.22. Andersen H, Gadeberg PC, Brock B, Jakobsen J. Muscular atrophy in diabetic neuropathy: a stereological magnetic resonance imaging study. Diabetologia. 1997; 40:1062–1069.23. Barazzoni R. Skeletal muscle mitochondrial protein metabolism and function in ageing and type 2 diabetes. Curr Opin Clin Nutr Metab Care. 2004; 7:97–102.24. Metter EJ, Lynch N, Conwit R, Lindle R, Tobin J, Hurley B. Muscle quality and age: cross-sectional and longitudinal comparisons. J Gerontol A Biol Sci Med Sci. 1999; 54:B207–B218.25. Newman AB, Haggerty CL, Goodpaster B, Harris T, Kritchevsky S, Nevitt M, Miles TP, Visser M. Health Aging And Body Composition Research Group. Strength and muscle quality in a well-functioning cohort of older adults: the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003; 51:323–330.26. Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006; 61:1059–1064.27. Alexander NB, Schultz AB, Warwick DN. Rising from a chair: effects of age and functional ability on performance biomechanics. J Gerontol. 1991; 46:M91–M98.28. Wolfson L, Judge J, Whipple R, King M. Strength is a major factor in balance, gait, and the occurrence of falls. J Gerontol A Biol Sci Med Sci. 1995; 50 Spec No:64–67.29. Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, Korytkowski MT, Munshi MN, Odegard PS, Pratley RE, Swift CS. Diabetes in older adults. Diabetes Care. 2012; 35:2650–2664.30. Lebovitz HE. American Diabetes Association. Charter 31, Diabetes in older adults. Therapy for diabetes mellitus and related disorders. 5th ed. Alexandria: American Diabetes Association;2009. p. 364–365.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
- Response: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
- Sarcopenia, Frailty, and Diabetes in Older Adults
- Gender Differences in the Link Between Marital Quality and Cognitive Decline Among Older Adults in Korea
- Management of Elderly Diabetes Patients Who Are Unable to Self-Care