J Korean Fract Soc.
2016 Apr;29(2):114-120. 10.12671/jkfs.2016.29.2.114.
Usefulness of Computed Tomography on Distal Tibia Intra-Articular Fracture Associated with Spiral Tibia Shaft Fracture
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 2Department of Orthopaedic Surgery, CHA Gumi Medical Center, CHA University, Gumi, Korea. bgkimmd@gmail.com
- KMID: 2162013
- DOI: http://doi.org/10.12671/jkfs.2016.29.2.114
Abstract
- PURPOSE
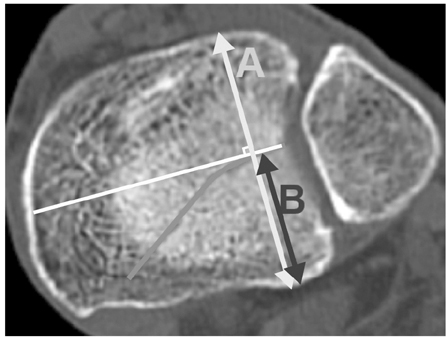
The purpose of this study is to evaluate the usefulness of computed tomography (CT) for spiral tibia shaft fracture by analyzing associated distal tibia intra-articular fractures diagnosed by CT only which met the indication of surgical fixation and were fixed.
MATERIALS AND METHODS
Ninety-five spiral tibia shaft fractures with preoperative ankle plain radiographs and CT were analyzed retrospectively. The incidence and type of associated distal tibia articular fractures were evaluated by reviewing ankle plain radiography and CT. The number of fractures diagnosed by CT that correspond with the indication of fixation and that were actually fixed were analyzed.
RESULTS
Among 95 spiral tibia shaft fractures, 62 cases (65.3%) were associated with distal tibia intra-articular fracture. There were 37 cases of posterior malleolar fracture, 5 cases of avulsion fracture of the distal anterior tibiofibular ligament, 5 cases of medial malleolar fracture, and 15 cases of complex fracture. Among 52 posterior malleolar fractures including complex fracture, 20 cases were diagnosed by ankle plain radiograph. Of these 20 cases, 16 posterior malleolar fractures (80.0%) met the indication of surgical fixation, and 14 cases were actually fixed with a screw. Among 32 posterior malleolar fractures diagnosed by CT only, 26 cases (81.3%) met the indication of surgical fixation and 18 cases (56.3%) were fixed by screw.
CONCLUSION
Approximately 50% of associated fractures were diagnosed by CT only and more than 80% of associated posterior malleolar fractures met the indication of surgical fixation and among these fractures, 18 cases (56.3%) were actually fixed by screw. This result suggests that CT is useful in diagnosis and treatment of distal tibia intra-articular fracture associated with spiral tibia shaft fracture.
MeSH Terms
Figure
Reference
-
1. Hou Z, Zhang Q, Zhang Y, Li S, Pan J, Wu H. A occult and regular combination injury: the posterior malleolar fracture associated with spiral tibial shaft fracture. J Trauma. 2009; 66:1385–1390.
Article2. Boraiah S, Gardner MJ, Helfet DL, Lorich DG. High association of posterior malleolus fractures with spiral distal tibial fractures. Clin Orthop Relat Res. 2008; 466:1692–1698.
Article3. Kukkonen J, Heikkilä JT, Kyyrönen T, Mattila K, Gullichsen E. Posterior malleolar fracture is often associated with spiral tibial diaphyseal fracture: a retrospective study. J Trauma. 2006; 60:1058–1060.
Article4. Purnell GJ, Glass ER, Altman DT, Sciulli RL, Muffly MT, Altman GT. Results of a computed tomography protocol evaluating distal third tibial shaft fractures to assess noncontiguous malleolar fractures. J Trauma. 2011; 71:163–168.
Article5. Schottel PC, Berkes MB, Little MT, et al. Predictive radiographic markers for concomitant ipsilateral ankle injuries in tibial shaft fractures. J Orthop Trauma. 2014; 28:103–107.
Article6. van der Werken C, Zeegers EV. Fracture of the lower leg with involvement of the posterior malleolus; a neglected combination? Injury. 1988; 19:241–243.
Article7. Georgiadis GM, Ebraheim NA, Hoeflinger MJ. Displacement of the posterior malleolus during intramedullary tibial nailing. J Trauma. 1996; 41:1056–1058.
Article8. Stuermer EK, Stuermer KM. Tibial shaft fracture and ankle joint injury. J Orthop Trauma. 2008; 22:107–112.
Article9. Kim JW, Choi HJ, Lee DH, Kim YC. Ankle fracture associated with tibia shaft fractures. J Korean Fract Soc. 2014; 27:136–143.
Article10. Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma. 1989; 29:1565–1570.11. Macko VW, Matthews LS, Zwirkoski P, Goldstein SA. The joint-contact area of the ankle. The contribution of the posterior malleolus. J Bone Joint Surg Am. 1991; 73:347–351.
Article12. Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br. 1995; 77:781–787.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ankle Fracture Associated with Tibia Shaft Fractures
- Assessment of Noncontiguous Posterior Malleolar Fractures in Distal One-Third Tibia Shaft Fractures with Proximal Fibula Fractures
- Extra-articular Triplane Fracture of Distal Tibial Physis - Report of a Case
- Relationship of Tibial Nonunion with Fibular Nonunion in the Tibio-fibular Shaft Fracture
- Pseudoaneurysm of the Anterior Tibial Artery after Reduction with Pointed Bone Reduction Forceps on a Spiral Fracture of the Distal Tibia: A Case Report