J Korean Soc Radiol.
2015 Mar;72(3):185-188. 10.3348/jksr.2015.72.3.185.
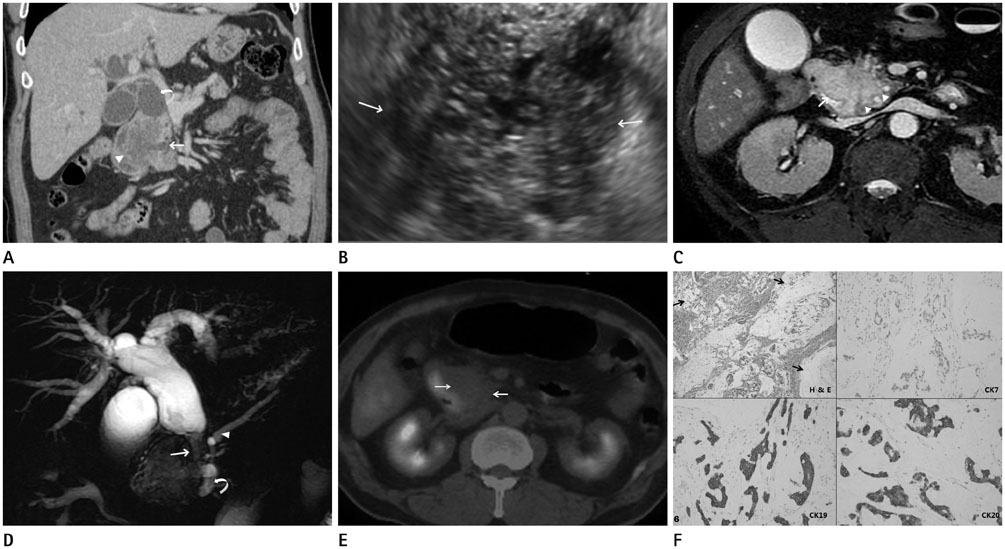
Duodenal Mucinous Carcinoma: A Case Report
- Affiliations
-
- 1Department of Radiology, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea. jkn1303@dreamwiz.com
- KMID: 2161171
- DOI: http://doi.org/10.3348/jksr.2015.72.3.185
Abstract
- Duodenal mucinous carcinoma is exceedingly rare and a case report about duodenal mucinous carcinoma in a 61-year-old man mimicking pancreatic cystic neoplasm by radiological evaluation, endoscopy, and even surgical findings is presented.
MeSH Terms
Figure
Reference
-
1. DiSario JA, Burt RW, Vargas H, McWhorter WP. Small bowel cancer: epidemiological and clinical characteristics from a population-based registry. Am J Gastroenterol. 1994; 89:699–701.2. Okumura F, Senoo K, Yoshida M, Miyabe K, Naito I, Tanaka H, et al. [A case of peritoneal dissemination from mucinous carcinoma of the duodenum, which was associated with tumor thrombosis in the accessory pancreatic duct and successfully treated by chemotherapy]. Nihon Shokakibyo Gakkai Zasshi. 2009; 106:1736–1743.3. Tsuro K, Matsumoto M, Moriyasu H, Nakatani Y, Sakurai S, Maekawa Y, et al. A case of duodenal mucinous adenocarcinoma infiltrating the cystic duct diagnosed as transpapillary with transnasal endoscopy. Dig Endosc. 2010; 22:246–247.4. Yagyu T, Aihara T, Murayama M, Kikuchi S, Nakamura E, Hase K, et al. Mucinous carcinoma of the duodenum associated with hereditary nonpolyposis colorectal cancer: report of a case. Surg Today. 2006; 36:1129–1132.5. Rosai J. Rosai and Ackerman's Surgical Pathology. In : Rosai J, editor. Gastrointestinal tract: esophagus, stomach, small bowel, appendix, large bowel, anus. 10th ed. Philadelphia: Elsevier-Mosby;2011. p. 731–755.6. Ko EY, Ha HK, Kim AY, Yoon KH, Yoo CS, Kim HC, et al. CT differentiation of mucinous and nonmucinous colorectal carcinoma. AJR Am J Roentgenol. 2007; 188:785–791.7. Hussain SM, Outwater EK, Siegelman ES. Mucinous versus nonmucinous rectal carcinomas: differentiation with MR imaging. Radiology. 1999; 213:79–85.8. Berger KL, Nicholson SA, Dehdashti F, Siegel BA. FDG PET evaluation of mucinous neoplasms: correlation of FDG uptake with histopathologic features. AJR Am J Roentgenol. 2000; 174:1005–1008.9. Itoh S, Ishiguchi T, Ishigaki T, Sakuma S, Maruyama K, Senda K. Mucin-producing pancreatic tumor: CT findings and histopathologic correlation. Radiology. 1992; 183:81–86.10. Kawamura H, Kondo Y, Osawa S, Nisida Y, Okada K, Isizu H, et al. A clinicopathologic study of mucinous adenocarcinoma of the stomach. Gastric Cancer. 2001; 4:83–86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Patient with Duodenal Mucinous Adenocarcinoma Presenting as a Laterally Spreading Tumor
- A Case of Cutaneous Mucinous Eccrine Carcinoma
- Ovarian Large Cell Neuroendocrine Carcinoma Associated with Endocervical-like Mucinous Borderline Tumor: A Case Report and Literature Review
- A Case of Cutaneous Mucinous Eccrine Carcinoma
- Mucocele-like Tumor of the Breast: A clinicopathologic case report