J Korean Soc Radiol.
2015 Mar;72(3):156-163. 10.3348/jksr.2015.72.3.156.
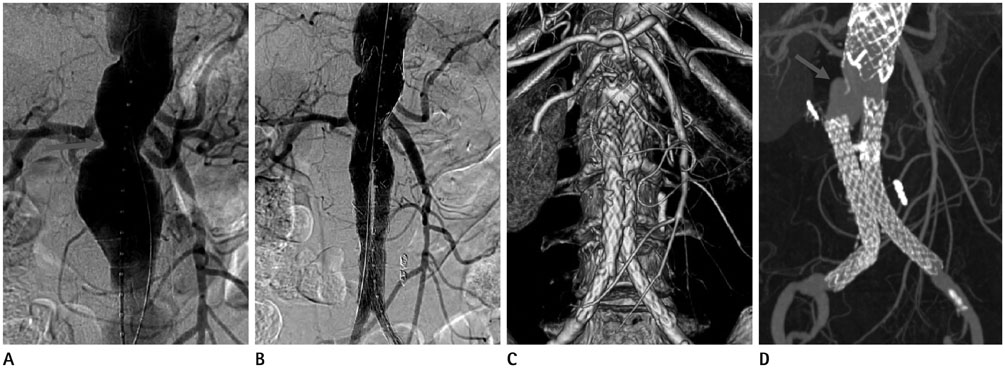
Endovascular Therapy for Abdominal Aortic Aneurysm and Iliac Artery Aneurysm Using SEAL Aortic Stent-Graft: A Single Center Experience
- Affiliations
-
- 1Department of Radiology, Gachon University Gil Hospital, Incheon, Korea. ho7ok7@gilhospital.com
- 2Department of Vascular Surgery, Gachon University Gil Hospital, Incheon, Korea.
- KMID: 2161166
- DOI: http://doi.org/10.3348/jksr.2015.72.3.156
Abstract
- PURPOSE
The aim of this study was to evaluate the safety and efficacy of SEAL aortic stent-graft for abdominal aortoiliac aneurysms.
MATERIALS AND METHODS
Between October 2007 and January 2014, 33 patients with abdominal aortoiliac aneurysms were treated with SEAL aortic stent-graft. We evaluated the technical success rate, clinical and CT follow-up periods, major complications, need for additional interventional treatment, aneurysm-related mortality and clinical success rate.
RESULTS
SEAL bifurcated aortic stent-graft was successfully placed in 32 patients (97%). Clinical and CT follow-up periods were 24 and 14 months, respectively. Endoleak developed in 13 patients (41%): spontaneous regression or decrease in 6, need for additional treatment in 4 and follow-up loss in 3. Significant stenosis of stent-graft occurred in 4 patients (12%) and was treated with stenting in 3. Migration of stent-graft was noted in 3 patients (9%) and treated with additional stent-grafting. Aneurysm-related mortality was 9% (3 of 33). The placement of SEAL stent-graft was effective in 26 patients (79%).
CONCLUSION
The placement of SEAL aortic stent-graft was safe and effective in patients with aneurysms of abdominal aorta and iliac arteries. However, complicating endoleaks, stenosis and migration of the stent-graft developed during the follow-up. Therefore, regular CT follow-up seems to be mandatory.
MeSH Terms
Figure
Reference
-
1. Brewster DC, Jones JE, Chung TK, Lamuraglia GM, Kwolek CJ, Watkins MT, et al. Long-term outcomes after endovascular abdominal aortic aneurysm repair: the first decade. Ann Surg. 2006; 244:426–438.2. Lee DY, Kang SG, Choi D, Lee GH, Maeda M, Roh BS, et al. Percutaneous modular stent-grafts in the treatment of abdominal aortic aneurysms. J Endovasc Ther. 2003; 10:752–759.3. You JH, Park HK, Park CB. Endovascular repair of bilateral iliac artery aneurysm with branched iliac stents: case report and review of the current literature. J Korean Surg Soc. 2013; 85:145–148.4. Chaikof EL, Fillinger MF, Matsumura JS, Rutherford RB, White GH, Blankensteijn JD, et al. Identifying and grading factors that modify the outcome of endovascular aortic aneurysm repair. J Vasc Surg. 2002; 35:1061–1066.5. Veith FJ, Baum RA, Ohki T, Amor M, Adiseshiah M, Blankensteijn JD, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002; 35:1029–1035.6. White GH, Yu W, May J. Endoleak--a proposed new terminology to describe incomplete aneurysm exclusion by an endoluminal graft. J Endovasc Surg. 1996; 3:124–125.7. White GH, May J, Waugh RC, Chaufour X, Yu W. Type III and type IV endoleak: toward a complete definition of blood flow in the sac after endoluminal AAA repair. J Endovasc Surg. 1998; 5:305–309.8. Katsargyris A, Botos B, Oikonomou K, Pedraza de Leistl M, Ritter W, Verhoeven EL. The new C3 Gore Excluder stent-graft: single-center experience with 100 patients. Eur J Vasc Endovasc Surg. 2014; 47:342–348.9. Iwakoshi S, Ichihashi S, Higashiura W, Itoh H, Sakaguchi S, Tabayashi N, et al. A decade of outcomes and predictors of sac enlargement after endovascular abdominal aortic aneurysm repair using zenith endografts in a Japanese population. J Vasc Interv Radiol. 2014; 25:694–701.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Stent-Graft Placement and Secondary Intervention for Abdominal Aortic Aneurysm in a Patient who had a Previously Inserted Iliac Stent
- Endovascular aortic aneurysm repair using a bifurcated stent graft in a patient with femoro-femoral bypass
- Endovascular Repair of Thoracic Aortic Aneurysm Using a Custom-made Fenestrated Stent Graft to Preserve the Left Subclavian Artery
- Successful Endovascular Management of Intraoperative Graft Limb Occlusion and Iliac Artery Rupture Occurred during Endovascular Abdominal Aortic Aneurysm Repair
- The Upside-Down Gore Excluder Limb and Double-Barrel Sandwich Technique for Penetrating Aortic Ulcer and Iliac Aneurysm Exclusion