J Gynecol Oncol.
2015 Jul;26(3):179-184. 10.3802/jgo.2015.26.3.179.
Role of vaginal pallor reaction in predicting late vaginal stenosis after high-dose-rate brachytherapy in treatment-naive patients with cervical cancer
- Affiliations
-
- 1Department of Radiology, Osaka Medical College, Takatsuki, Japan.
- 2Department of Radiology, Kyoto Prefectural University of Medicine, Kyoto, Japan. hideya10@hotmail.com
- 3Department of Radiology, National Hospital Organization Osaka National Hospital, Osaka, Japan.
- 4Department of Radiation Oncology, Osaka University Graduate School of Medicine, Osaka, Japan.
- KMID: 2160803
- DOI: http://doi.org/10.3802/jgo.2015.26.3.179
Abstract
OBJECTIVE
To assess actual rates of late vaginal stenosis and identify predisposing factors for complications among patients with previously untreated cervical cancer following high-dose-rate brachytherapy.
METHODS
We performed longitudinal analyses of 57 patients using the modified Dische score at 6, 12, 18, 24, 36, and 60 months after treatment, which consisted of 15 interstitial brachytherapys and 42 conventional intracavitary brachytherapys, with a median follow-up time of 36 months (range, 6 to 144 months).
RESULTS
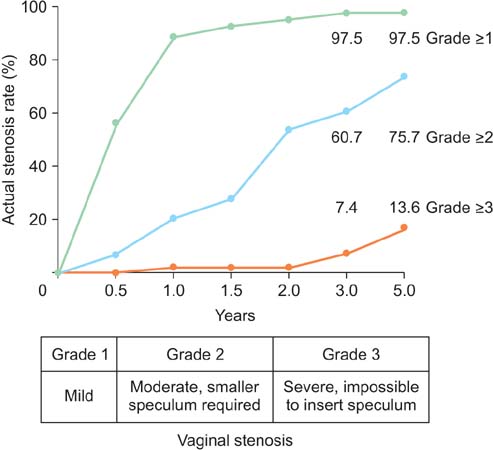
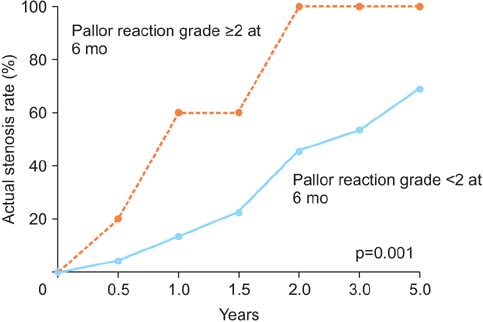
More than half of the patients developed grade 1 (mild) vaginal stenosis within the first year of follow-up, and grade 2 (97.5%, moderate) to grade 3 (severe) stenosis gradually increased with time. Actual stenosis rates for grade 1, 2, and 3 were 97.5% (95% confidence interval [CI], 92.7 to 97.5), 60.7% (95% CI, 42.2 to 79.3), and 7.4% (95% CI, 0 to 18.4) at 3 years after treatment. Pallor reaction grade 2-3 at 6 months was only a statistically significant predisposing factor for grade 2-3 late vaginal stenosis 3 years or later with a hazard ratio of 3.48 (95% CI, 1.32 to 9.19; p=0.018) by a multivariate Cox proportional hazard model. Patients with grade 0-1 pallor reaction at 6 months showed a grade > or =2 vaginal stenosis rate of 53%, whereas the grade 2-3 pallor reaction group achieved a grade > or =2 vaginal stenosis rate at 3 years at 100% (p=0.001).
CONCLUSION
High-dose-rate brachytherapy was associated with high incidence of late vaginal stenosis. Pallor reaction grade 2-3 at 6 months was predictive of late grade 2-3 vaginal stenosis at 3 years after treatment. These findings should prove helpful for patient counseling and preventive intervention.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Brachytherapy/*adverse effects/methods
Constriction, Pathologic/etiology/pathology
Female
Humans
Iridium Radioisotopes/therapeutic use
Middle Aged
*Pallor
Prognosis
Prospective Studies
Radiopharmaceuticals/therapeutic use
Retrospective Studies
Uterine Cervical Neoplasms/*radiotherapy
Vaginal Diseases/*etiology/pathology
Iridium Radioisotopes
Radiopharmaceuticals
Figure
Reference
-
1. Barbera L, Thomas G. Management of early and locally advanced cervical cancer. Semin Oncol. 2009; 36:155–169.2. Gondi V, Bentzen SM, Sklenar KL, Dunn EF, Petereit DG, Tannehill SP, et al. Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: an inter-era analysis. Int J Radiat Oncol Biol Phys. 2012; 84:973–982.3. Teshima T, Inoue T, Ikeda H, Miyata Y, Nishiyama K, Inoue T, et al. High-dose rate and low-dose rate intracavitary therapy for carcinoma of the uterine cervix. Final results of Osaka University Hospital. Cancer. 1993; 72:2409–2414.4. Toita T, Kitagawa R, Hamano T, Umayahara K, Hirashima Y, Aoki Y, et al. Phase II study of concurrent chemoradiotherapy with high-dose-rate intracavitary brachytherapy in patients with locally advanced uterine cervical cancer: efficacy and toxicity of a low cumulative radiation dose schedule. Gynecol Oncol. 2012; 126:211–216.5. Yoshida K, Yamazaki H, Nakamura S, Masui K, Kotsuma T, Baek SJ, et al. Comparisons of late vaginal mucosal reactions between interstitial and conventional intracavitary brachytherapy in patients with gynecological cancer: speculation on the relation between pallor reaction and stenosis. Anticancer Res. 2013; 33:3963–3968.6. Yoshida K, Yamazaki H, Nakamura S, Masui K, Kotsuma T, Akiyama H, et al. Longitudinal analysis of late vaginal mucosal reactions after high-dose-rate brachytherapy in patients with gynecological cancer. Anticancer Res. 2014; 34:4433–4438.7. Kirchheiner K, Nout RA, Tanderup K, Lindegaard JC, Westerveld H, Haie-Meder C, et al. Manifestation pattern of early-late vaginal morbidity after definitive radiation (chemo)therapy and image-guided adaptive brachytherapy for locally advanced cervical cancer: an analysis from the EMBRACE study. Int J Radiat Oncol Biol Phys. 2014; 89:88–95.8. Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev. 2010; (9):CD007291.9. Yoshida K, Yamazaki H, Takenaka T, Kotsuma T, Yoshida M, Furuya S, et al. A dose-volume analysis of magnetic resonance imaging-aided high-dose-rate image-based interstitial brachytherapy for uterine cervical cancer. Int J Radiat Oncol Biol Phys. 2010; 77:765–772.10. Yamazaki H, Inoue T, Ikeda H, Tang JT, Murayama S, Teshima T, et al. High-dose-rate remote afterloading intestinal radiotherapy employing the template technique for recurrent cancer in the pelvic area. Strahlenther Onkol. 1993; 169:481–485.11. Bruner DW, Lanciano R, Keegan M, Corn B, Martin E, Hanks GE. Vaginal stenosis and sexual function following intracavitary radiation for the treatment of cervical and endometrial carcinoma. Int J Radiat Oncol Biol Phys. 1993; 27:825–830.12. Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2003; 56:937–949.13. Bakker RM, Vermeer WM, Creutzberg CL, Mens JW, Nout RA, Ter Kuile MM. Qualitative accounts of patients' determinants of vaginal dilator use after pelvic radiotherapy. J Sex Med. 2015; 12:764–773.14. Bahng AY, Dagan A, Bruner DW, Lin LL. Determination of prognostic factors for vaginal mucosal toxicity associated with intravaginal high-dose rate brachytherapy in patients with endometrial cancer. Int J Radiat Oncol Biol Phys. 2012; 82:667–673.15. Fidarova EF, Berger D, Schussler S, Dimopoulos J, Kirisits C, Georg P, et al. Dose volume parameter D2cc does not correlate with vaginal side effects in individual patients with cervical cancer treated within a defined treatment protocol with very high brachytherapy doses. Radiother Oncol. 2010; 97:76–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Design of a New Applicator for High-Dose Rate Vaginal Brachytherapy
- Dosimetric analysis of intracavitary brachytherapy applicators: a practical study
- High-Dose-Rate Brachytherapy for the Treatment of Vaginal Intraepithelial Neoplasia
- Radiation sigmoiditis mimicking sigmoid colon cancer after radiation therapy for cervical cancer: the implications of three-dimensional image-based brachytherapy planning
- Air in Vagina: Significance in the Staging of Uterine Cervical Carcinoma