Korean J Ophthalmol.
2016 Apr;30(2):108-113. 10.3341/kjo.2016.30.2.108.
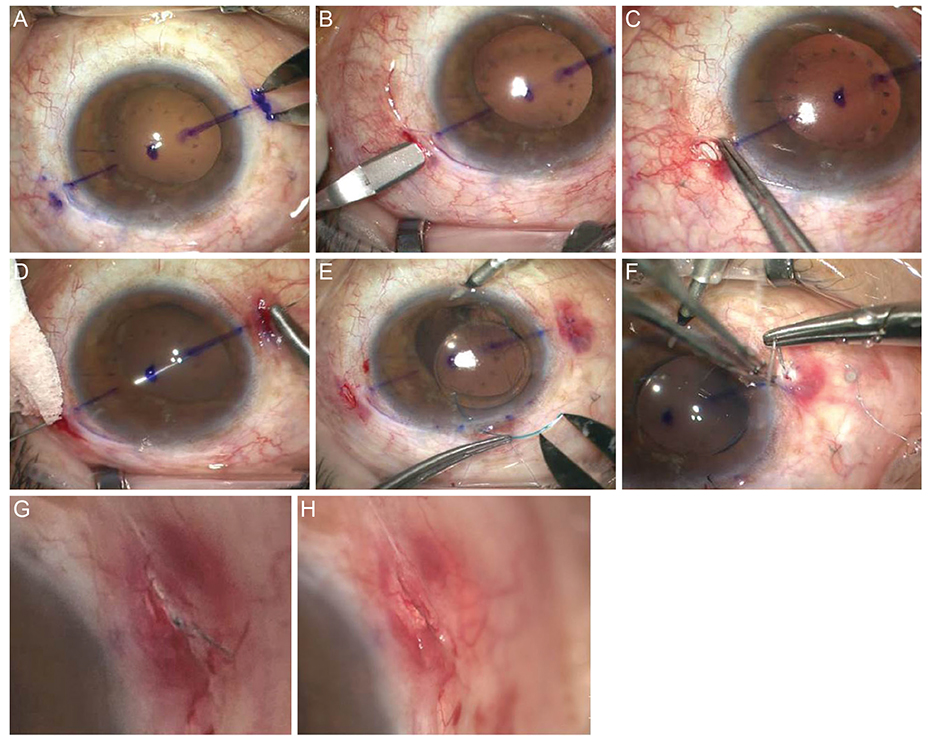
Short-term Clinical Outcomes after Transscleral Fixation Using the Intrascleral Pocket Technique: A Retrospective Cohort Study Analysis
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University College of Medicine, Jinju, Korea. maya12kim@naver.com
- 2Gyeongsang Institute of Health Science, Gyeongsang National University, Jinju, Korea.
- KMID: 2160460
- DOI: http://doi.org/10.3341/kjo.2016.30.2.108
Abstract
- PURPOSE
To compare the two transscleral fixation (TSF) techniques of intrascleral pocket and conventional scleral flap with conjunctival division techniques in terms of short-term clinical effects.
METHODS
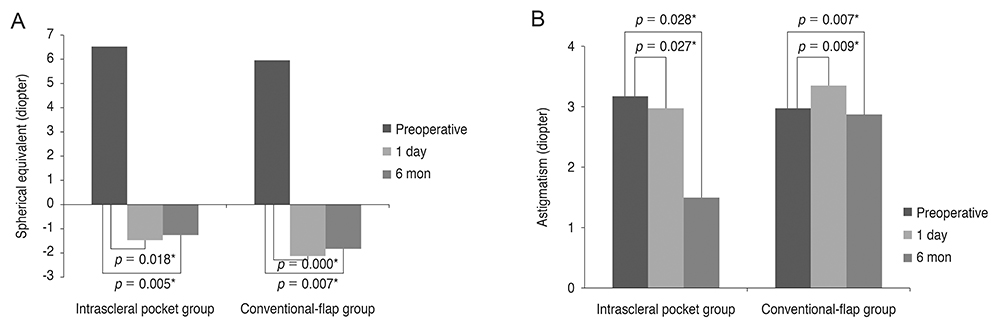
This retrospective cohort study included all consecutive patients with aphakia in Gyeongsang National University Hospital in Jinju, Korea, who underwent TSF between January 2012 and December 2014. The medical records of all patients were retrospectively reviewed, and the endothelial cell count (ECC), refraction, best-corrected visual acuity (BCVA), intraocular pressure, slit lamp, and fundus examination results before and 1 day and 6 months after surgery were recorded. The postoperative complications and visual outcomes were also recorded.
RESULTS
The intrascleral pocket and conventional-flap groups did not differ significantly in terms of demographics, presurgical BCVA, or ECC. However, the intrascleral pocket group had a significantly lower BCVA at 1 day and 6 months after surgery compared to the conventional-flap group. The two groups did not differ in terms of ECC 6 months after surgery. The intrascleral pocket group had no postoperative complications, but five patients in the conventional-flap group complained of irritation. In both groups, the intraocular lens was well positioned without tilting or subluxation, and astigmatism was significantly reduced at 1 day and 6 months after surgery.
CONCLUSIONS
The intrascleral pocket technique of TSF does not involve conjunctival dissection and is a successful method of sulcus fixation. It stably corrects the intraocular lens and is easy to perform, which helps to reduce operation time. It also reliably yields rapid visual acuity recovery without complications.
MeSH Terms
Figure
Reference
-
1. Wagoner MD, Cox TA, Ariyasu RG, et al. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003; 110:840–859.2. Lewis JS. Ab externo sulcus fixation. Ophthalmic Surg. 1991; 22:692–695.3. Teichmann KD. Pars plana fixation of posterior chamber intraocular lenses. Ophthalmic Surg. 1994; 25:549–553.4. Kim DH, Heo JW, Hwang SW, et al. Modified transscleral fixation using combined temporary haptic externalization and injector intraocular lens implantation. J Cataract Refract Surg. 2010; 36:707–711.5. Ma DJ, Kim MK, Wee WR. Knotless external fixation technique for posterior chamber intraocular lens transscleral fixation: a 5-case analysis. J Korean Ophthalmol Soc. 2012; 53:1609–1614.6. Lin CP, Tseng HY. Suture fixation technique for posterior chamber intraocular lenses. J Cataract Refract Surg. 2004; 30:1401–1404.7. Solomon K, Gussler JR, Gussler C, Van Meter WS. Incidence and management of complications of transsclerally sutured posterior chamber lenses. J Cataract Refract Surg. 1993; 19:488–493.8. Lewis JS. Sulcus fixation without flaps. Ophthalmology. 1993; 100:1346–1350.9. Kir E, Kocaturk T, Dayanir V, et al. Prevention of suture exposure in transscleral intraocular lens fixation: an original technique. Can J Ophthalmol. 2008; 43:707–711.10. Cho YW, Chung IY, Yoo JM, Kim SJ. Sutureless intrascleral pocket technique of transscleral fixation of intraocular lens in previous vitrectomized eyes. Korean J Ophthalmol. 2014; 28:181–185.11. Malbran ES, Malbran E Jr, Negri I. Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction. Int Ophthalmol. 1986; 9:151–160.12. Szurman P, Petermeier K, Aisenbrey S, et al. Z-suture: a new knotless technique for transscleral suture fixation of intraocular implants. Br J Ophthalmol. 2010; 94:167–169.13. Stewart MW, Landers MB 3rd. Transscleral intraocular lens fixation with a "homemade" needle and hook. J Cataract Refract Surg. 2006; 32:200–202.14. Heilskov T, Joondeph BC, Olsen KR, Blankenship GW. Late endophthalmitis after transscleral fixation of a posterior chamber intraocular lens. Arch Ophthalmol. 1989; 107:1427.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sutureless Intrascleral Pocket Technique of Transscleral Fixation of Intraocular Lens in Previous Vitrectomized Eyes
- Short-term Clinical Outcomes after Flanged Intrascleral Fixation of Intraocular Lenses Using Oblique Intrascleral Tunnels
- Clinical Outcomes of Intrascleral Fixation of Intraocular Lens Compared to Ciliary Sulcus Implantation and Transscleral Fixation
- Short-Term Comparison of Surgical Results between One-Haptic and Two-Haptics Transscleral Fixation of Intraocular Lens
- Is This Really Sutureless Intrascleral Pocket Technique of Transscleral Fixation?