Korean J Ophthalmol.
2016 Apr;30(2):92-100. 10.3341/kjo.2016.30.2.92.
Factors Affecting Long-term Myopic Regression after Laser In Situ Keratomileusis and Laser-assisted Subepithelial Keratectomy for Moderate Myopia
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- 2Department of Ophthalmology, Ewha Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Yeouido St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2160458
- DOI: http://doi.org/10.3341/kjo.2016.30.2.92
Abstract
- PURPOSE
High myopia is known to be a risk factor for long-term regression after laser refractive surgery. There have been few studies about the correction of moderate myopias that did not need retreatment after long-term follow-up. We evaluated 10 years of change in visual acuity and refractive power in eyes with moderate myopia after laser refractive surgery.
METHODS
We included patients that had undergone laser in situ keratomileusis (LASIK) or laser-assisted subepithelial keratectomy (LASEK) to correct their myopia and that had at least 10 years of follow-up. We evaluated the stability of visual acuity in terms of safety, efficacy, and refractive changes at examinations 6 months and 1, 2, 5, 7, and 10 years after surgery.
RESULTS
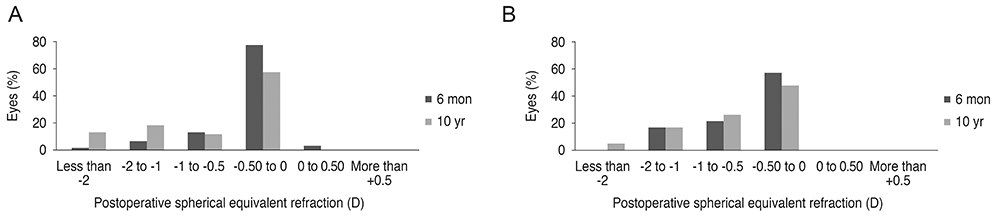
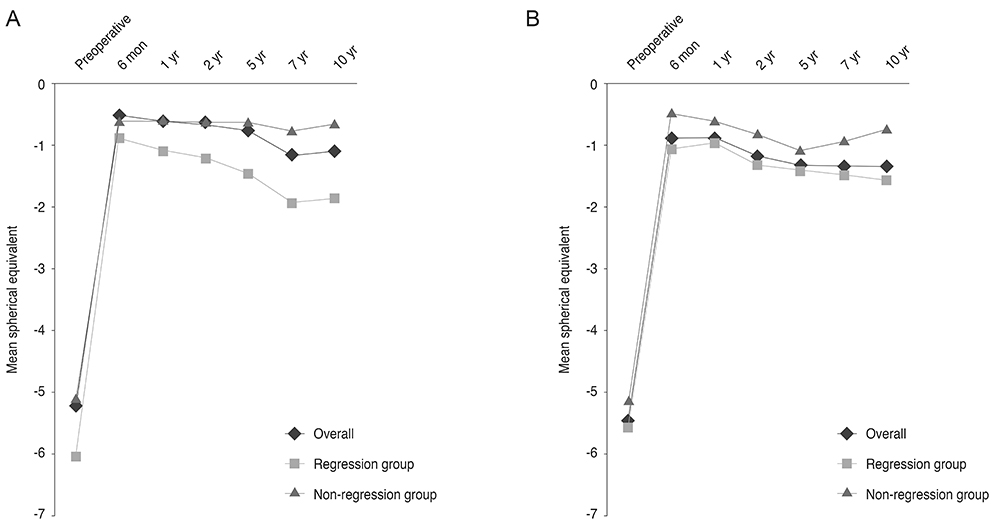
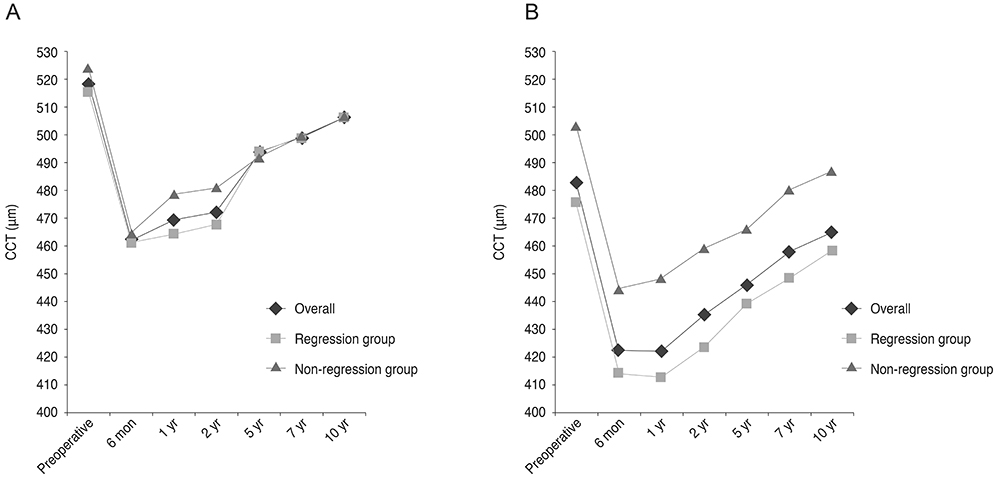
The study evaluated 62 eyes (36 eyes in LASIK patients and 26 eyes in LASEK patients). In both groups, the efficacy index tended to decrease, and it was consistently higher in the LASEK group compared to the LASIK group over the 10 years of follow-up. The safety index improved over 10 years and was always higher than 0.9 in both groups. The difference between the spherical equivalent at 6 months postoperatively and later periods was statistically significant after 5, 7, and 10 years in both groups (LASIK, p = 0.036, p = 0.003, and p < 0.001, respectively; LASEK, p = 0.006, p = 0.002, and p = 0.001, respectively). Ten years after surgery,26 eyes (66.7%) in the LASIK group and 19 eyes (73.1%) in the LASEK group had myopia greater than 1 diopter. In comparison with the thickness at 6 months postoperatively, central corneal thickness was significantly increased after 5, 7, and 10 years in both LASIK and LASEK groups (LASIK, p < 0.001, p < 0.001, and p < 0.001, respectively; LASEK, p = 0.01, p < 0.001, and p < 0.001, respectively).
CONCLUSIONS
Moderately myopic eyes showed progressive myopic shifting and corneal thickening after LASIK and LASEK during 10 years of follow-up. We also found that early refractive regression may indicate the long-term refractive outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Chayet AS, Assil KK, Montes M, et al. Regression and its mechanisms after laser in situ keratomileusis in moderate and high myopia. Ophthalmology. 1998; 105:1194–1199.2. Pang G, Zhan S, Li Y, et al. Myopic regression after photorefractive keratectomy. Zhonghua Yan Ke Za Zhi. 1998; 34:451–453.3. Alio JL, Soria F, Abbouda A, Pena-Garcia P. Laser in situ keratomileusis for -6.00 to -18.00 diopters of myopia and up to -5.00 diopters of astigmatism: 15-year follow-up. J Cataract Refract Surg. 2015; 41:33–40.4. Lin MY, Chang DC, Hsu WM, Wang IJ. Cox proportional hazards model of myopic regression for laser in situ keratomileusis flap creation with a femtosecond laser and with a mechanical microkeratome. J Cataract Refract Surg. 2012; 38:992–999.5. Kim G, Christiansen SM, Moshirfar M. Change in keratometry after myopic laser in situ keratomileusis and photorefractive keratectomy. J Cataract Refract Surg. 2014; 40:564–574.6. Seiler T. Current evaluation of myopia correction with the excimer laser. Ophthalmologe. 1995; 92:379–384.7. Sutton GL, Kim P. Laser in situ keratomileusis in 2010: a review. Clin Experiment Ophthalmol. 2010; 38:192–210.8. Hammond MD, Madigan WP Jr, Bower KS. Refractive surgery in the United States Army, 2000-2003. Ophthalmology. 2005; 112:184–190.9. Tobaigy FM, Ghanem RC, Sayegh RR, et al. A control-matched comparison of laser epithelial keratomileusis and laser in situ keratomileusis for low to moderate myopia. Am J Ophthalmol. 2006; 142:901–908.10. Scerrati E. Laser in situ keratomileusis vs. laser epithelial keratomileusis (LASIK vs. LASEK). J Refract Surg. 2001; 17:2 Suppl. S219–S221.11. Kim JK, Kim SS, Lee HK, et al. Laser in situ keratomileusis versus laser-assisted subepithelial keratectomy for the correction of high myopia. J Cataract Refract Surg. 2004; 30:1405–1411.12. Liu HQ, Shi JP, Ma CR, et al. Multifactor analysis of the reasons causing undercorrection after laser in situ keratomileusis. Zhonghua Liu Xing Bing Xue Za Zhi. 2003; 24:307–309.13. Pan Q, Gu YS, Wang J, et al. Differences between regressive eyes and non-regressive eyes after LASIK for myopia in the time course of corneal changes assessed with the Orbscan. Ophthalmologica. 2004; 218:96–101.14. Netto MV, Mohan RR, Ambrosio R Jr, et al. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea. 2005; 24:509–522.15. O'Connor J, O'Keeffe M, Condon PI. Twelve-year follow-up of photorefractive keratectomy for low to moderate myopia. J Refract Surg. 2006; 22:871–877.16. O'Doherty M, O'Keeffe M, Kelleher C. Five year follow up of laser in situ keratomileusis for all levels of myopia. Br J Ophthalmol. 2006; 90:20–23.17. Reinstein DZ, Srivannaboon S, Gobbe M, et al. Epithelial thickness profile changes induced by myopic LASIK as measured by Artemis very high-frequency digital ultrasound. J Refract Surg. 2009; 25:444–450.18. Hirsch MJ. Relation of visual acuity to myopia. Arch Ophthal. 1945; 34:418–421.19. Wood PH. Appreciating the consequences of disease: the international classification of impairments, disabilities, and handicaps. WHO Chron. 1980; 34:376–380.20. Wang Z, Chen J, Yang B. Posterior corneal surface topographic changes after laser in situ keratomileusis are related to residual corneal bed thickness. Ophthalmology. 1999; 106:406–409.21. Erie JC, Patel SV, McLaren JW, et al. Effect of myopic laser in situ keratomileusis on epithelial and stromal thickness: a confocal microscopy study. Ophthalmology. 2002; 109:1447–1452.22. Dirani M, Couper T, Yau J, et al. Long-term refractive outcomes and stability after excimer laser surgery for myopia. J Cataract Refract Surg. 2010; 36:1709–1717.23. de Benito-Llopis L, Alio JL, Ortiz D, et al. Ten-year follow-up of excimer laser surface ablation for myopia in thin corneas. Am J Ophthalmol. 2009; 147:768–773.e1-2.24. Randleman JB, Caster AI, Banning CS, Stulting RD. Corneal ectasia after photorefractive keratectomy. J Cataract Refract Surg. 2006; 32:1395–1398.25. Reinstein DZ, Ameline B, Puech M, et al. VHF digital ultrasound three-dimensional scanning in the diagnosis of myopic regression after corneal refractive surgery. J Refract Surg. 2005; 21:480–484.26. Spadea L, Fasciani R, Necozione S, Balestrazzi E. Role of the corneal epithelium in refractive changes following laser in situ keratomileusis for high myopia. J Refract Surg. 2000; 16:133–139.27. Lohmann CP, Guell JL. Regression after LASIK for the treatment of myopia: the role of the corneal epithelium. Semin Ophthalmol. 1998; 13:79–82.28. Magallanes R, Shah S, Zadok D, et al. Stability after laser in situ keratomileusis in moderately and extremely myopic eyes. J Cataract Refract Surg. 2001; 27:1007–1012.29. Dierick HG, Missotten L. Is the corneal contour influenced by a tension in the superficial epithelial cells? A new hypothesis? Refract Corneal Surg. 1992; 8:54–59.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coniparision of Clinical Results Between Keratomileusis In Situ and Laser Assisted In Situ Keratomileusis for High Myopia from -15 Diopter to -23 Diopter
- Short Term Clinical Results of Laser Epithelial Keratomileusis and Epi-Laser in Situ Keratomileusis for Moderate and High Myopia
- The Effect of Anti-glaucoma Eyedrops and 0.1% Fluorometholone on Myopic Regression after LASIK or LASEK
- Ocular deviation after unilateral laser in situ keratomileusis
- Laser in Situ Keratomileusis to Treat Low to Moderate Myopia