Yonsei Med J.
2013 Jul;54(4):1006-1014. 10.3349/ymj.2013.54.4.1006.
Femoral Graft-Tunnel Angles in Posterior Cruciate Ligament Reconstruction: Analysis with 3-Dimensional Models and Cadaveric Experiments
- Affiliations
-
- 1Department of Orthopaedic Surgery, Arthroscopy and Joint Research Institute, Yonsei University College of Medicine, Seoul, Korea. orthohwan@gmail.com
- KMID: 2158238
- DOI: http://doi.org/10.3349/ymj.2013.54.4.1006
Abstract
- PURPOSE
The purpose of this study was to compare four graft-tunnel angles (GTA), the femoral GTA formed by three different femoral tunneling techniques (the outside-in, a modified inside-out technique in the posterior sag position with knee hyperflexion, and the conventional inside-out technique) and the tibia GTA in 3-dimensional (3D) knee flexion models, as well as to examine the influence of femoral tunneling techniques on the contact pressure between the intra-articular aperture of the femoral tunnel and the graft.
MATERIALS AND METHODS
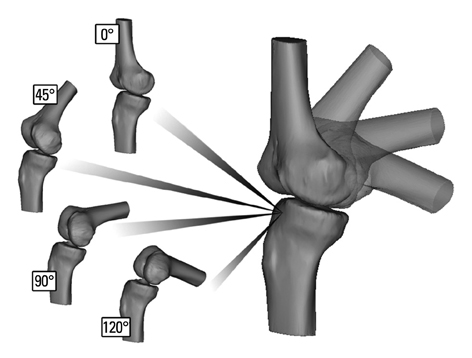
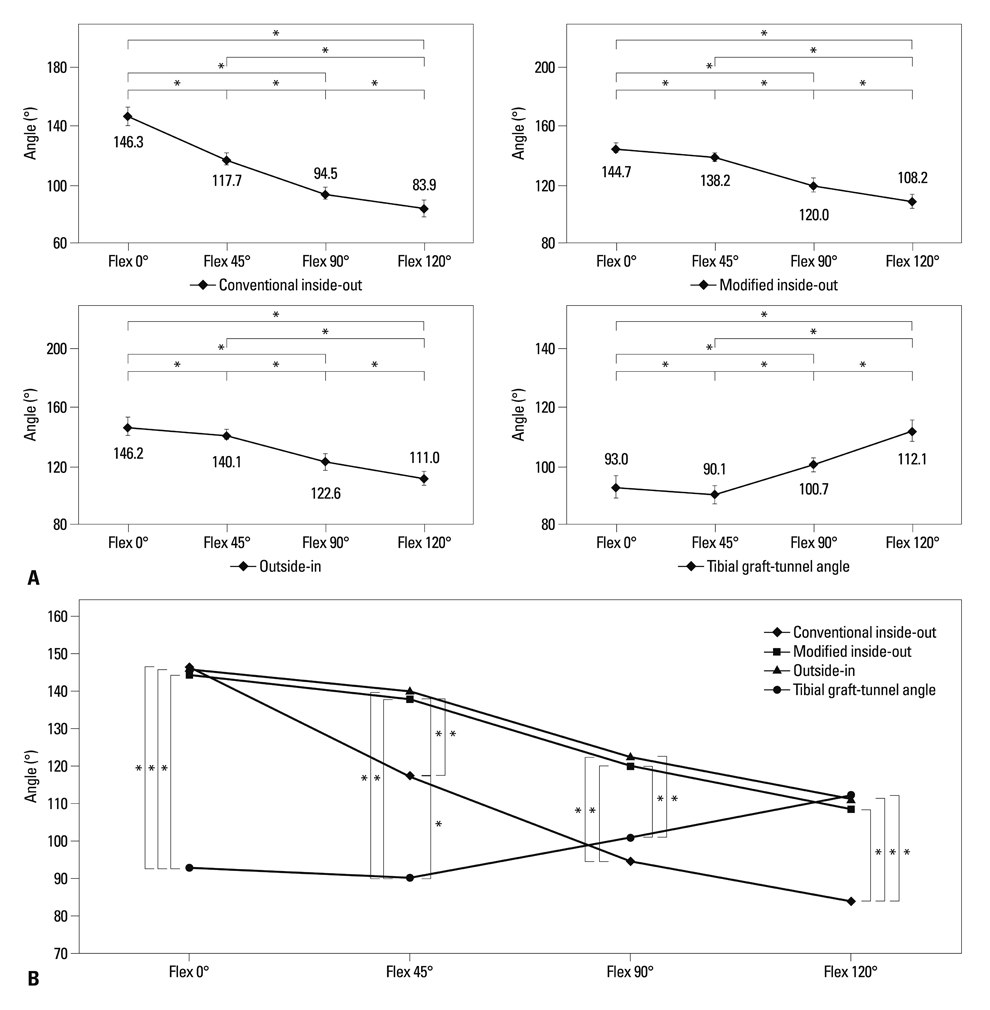
Twelve cadaveric knees were tested. Computed tomography scans were performed at different knee flexion angles (0degrees, 45degrees, 90degrees, and 120degrees). Femoral and tibial GTAs were measured at different knee flexion angles on the 3D knee models. Using pressure sensitive films, stress on the graft of the angulation of the femoral tunnel aperture was measured in posterior cruciate ligament reconstructed cadaveric knees.
RESULTS
Between 45degrees and 120degrees of knee flexion, there were no significant differences between the outside-in and modified inside-out techniques. However, the femoral GTA for the conventional inside-out technique was significantly less than that for the other two techniques (p<0.001). In cadaveric experiments using pressure-sensitive film, the maximum contact pressure for the modified inside-out and outside-in technique was significantly lower than that for the conventional inside-out technique (p=0.024 and p=0.017).
CONCLUSION
The conventional inside-out technique results in a significantly lesser GTA and higher stress at the intra-articular aperture of the femoral tunnel than the outside-in technique. However, the results for the modified inside-out technique are similar to those for the outside-in technique.
MeSH Terms
Figure
Reference
-
1. McAllister DR, Miller MD, Sekiya JK, Wojtys EM. Posterior cruciate ligament biomechanics and options for surgical treatment. Instr Course Lect. 2009; 58:377–388.2. Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med. 2001; 29:129–136.
Article3. Markolf KL, Zemanovic JR, McAllister DR. Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am. 2002; 84-A:518–524.
Article4. Kim SJ, Shin JW, Lee CH, Shin HJ, Kim SH, Jeong JH, et al. Biomechanical comparisons of three different tibial tunnel directions in posterior cruciate ligament reconstruction. Arthroscopy. 2005; 21:286–293.
Article5. Dunlop DG, Woodnutt DJ, Nutton RW. A new method to determine graft angles after knee ligament reconstruction. Knee. 2004; 11:19–24.
Article6. Handy MH, Blessey PB, Kline AJ, Miller MD. The graft/tunnel angles in posterior cruciate ligament reconstruction: a cadaveric comparison of two techniques for femoral tunnel placement. Arthroscopy. 2005; 21:711–714.
Article7. Schoderbek RJ Jr, Golish SR, Rubino LJ, Oliviero JA, Hart JM, Miller MD. The graft/femoral tunnel angles in posterior cruciate ligament reconstruction: a comparison of 3 techniques for femoral tunnel placement. J Knee Surg. 2009; 22:106–110.
Article8. Kim SJ, Min BH. Arthroscopic intraarticular interference screw technique of posterior cruciate ligament reconstruction: one-incision technique. Arthroscopy. 1994; 10:319–323.
Article9. Shino K, Nakagawa S, Nakamura N, Matsumoto N, Toritsuka Y, Natsu-ume T. Arthroscopic posterior cruciate ligament reconstruction using hamstring tendons: one-incision technique with Endobutton. Arthroscopy. 1996; 12:638–642.
Article10. Kim SJ, Kim HK, Kim HJ. A modified endoscopic technique for posterior cruciate ligament reconstruction using allograft. Arthroscopy. 1998; 14:643–648.
Article11. Kim SJ, Shin SJ, Kim HK, Jahng JS, Kim HS. Comparison of 1- and 2-incision posterior cruciate ligament reconstructions. Arthroscopy. 2000; 16:268–278.12. Tuan HS, Hutmacher DW. Application of micro CT and computation modeling in bone tissue engineering. Comput Aided Des. 2005; 37:1151–1161.
Article13. Victor J, Van Doninck D, Labey L, Innocenti B, Parizel PM, Bellemans J. How precise can bony landmarks be determined on a CT scan of the knee? Knee. 2009; 16:358–365.
Article14. Apsingi S, Bull AM, Deehan DJ, Amis AA. Review: femoral tunnel placement for PCL reconstruction in relation to the PCL fibre bundle attachments. Knee Surg Sports Traumatol Arthrosc. 2009; 17:652–659.
Article15. Lee YS, Ra HJ, Ahn JH, Ha JK, Kim JG. Posterior cruciate ligament tibial insertion anatomy and implications for tibial tunnel placement. Arthroscopy. 2011; 27:182–187.
Article16. Pearsall AW 4TH, Pyevich M, Draganich LF, Larkin JJ, Reider B. In vitro study of knee stability after posterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1996; 264–271.
Article17. Burns WC 2nd, Draganich LF, Pyevich M, Reider B. The effect of femoral tunnel position and graft tensioning technique on posterior laxity of the posterior cruciate ligament-reconstructed knee. Am J Sports Med. 1995; 23:424–430.
Article18. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008; 90:1922–1931.
Article19. Iriuchishima T, Tajima G, Ingham SJ, Shen W, Smolinski P, Fu FH. Impingement pressure in the anatomical and nonanatomical anterior cruciate ligament reconstruction: a cadaver study. Am J Sports Med. 2010; 38:1611–1617.
Article20. Natsu-ume T, Shino K, Nakata K, Nakamura N, Toritsuka Y, Mae T. Endoscopic reconstruction of the anterior cruciate ligament with quadrupled hamstring tendons. A correlation between MRI changes and restored stability of the knee. J Bone Joint Surg Br. 2001; 83:834–837.21. Toritsuka Y, Shino K, Horibe S, Mitsuoka T, Hamada M, Nakata K, et al. Second-look arthroscopy of anterior cruciate ligament grafts with multistranded hamstring tendons. Arthroscopy. 2004; 20:287–293.
Article22. Segawa H, Koga Y, Omori G, Sakamoto M, Hara T. Influence of the femoral tunnel location and angle on the contact pressure in the femoral tunnel in anterior cruciate ligament reconstruction. Am J Sports Med. 2003; 31:444–448.
Article23. Shearn JT, Grood ES, Noyes FR, Levy MS. One- and two-strand posterior cruciate ligament reconstructions: cyclic fatigue testing. J Orthop Res. 2005; 23:958–963.
Article24. Ohkoshi Y, Nagasaki S, Yamamoto K, Urushibara M, Tada H, Shigenobu K, et al. A new endoscopic posterior cruciate ligament reconstruction: minimization of graft angulation. Arthroscopy. 2001; 17:258–263.25. Kim SJ, Chang JH, Kang YH, Song DH, Park KY. Clinical comparison of anteromedial versus anterolateral tibial tunnel direction for transtibial posterior cruciate ligament reconstruction: 2 to 8 years' follow-up. Am J Sports Med. 2009; 37:693–698.
Article26. Nishimoto K, Kuroda R, Mizuno K, Hoshino Y, Nagamune K, Kubo S, et al. Analysis of the graft bending angle at the femoral tunnel aperture in anatomic double bundle anterior cruciate ligament reconstruction: a comparison of the transtibial and the far anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc. 2009; 17:270–276.
Article27. Papannagari R, DeFrate LE, Nha KW, Moses JM, Moussa M, Gill TJ, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med. 2007; 35:1507–1512.
Article28. Jeong WS, Yoo YS, Kim DY, Shetty NS, Smolinski P, Logishetty K, et al. An analysis of the posterior cruciate ligament isometric position using an in vivo 3-dimensional computed tomography-based knee joint model. Arthroscopy. 2010; 26:1333–1339.
Article29. Kim HY, Seo YJ, Kim HJ, Nguyenn T, Shetty NS, Yoo YS. Tension changes within the bundles of anatomic double-bundle anterior cruciate ligament reconstruction at different knee flexion angles: a study using a 3-dimensional finite element model. Arthroscopy. 2011; 27:1400–1408.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preparation of the Femoral Tunnel through Anteromedial Portal during Arthroscopic Single Incision Anterior Cruciate Ligament Reconstruction
- Optimal Orientation of the Femoral Tunnel in Reconstruction of Posterior Cruciate Ligament
- Arthrocopic Reconstruction of the Posterior Cruciate Ligment: The Effects of femoral attachment points and knee flexion angles at the time of graft fixation on posterior stability
- Three-Dimensional Reconstruction Computed Tomography Evaluation of the Tunnel Location and Angle in Anatomic Single-Bundle Anterior Cruciate Ligament Reconstruction: A Comparison of the Anteromedial Portal and Outside-in Techniques
- Effect of Anteromedial Portal Entrance Drilling Angle during Anterior Cruciate Ligament Reconstruction: A Three-Dimensional Computer Simulation