J Korean Med Sci.
2012 Jul;27(7):814-817. 10.3346/jkms.2012.27.7.814.
Kidney Transplantation in a Patient with End Stage Renal Disease after Complete Remission of Acute Promyelocytic Leukemia
- Affiliations
-
- 1Transplant Research Center, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea. yangch@catholic.ac.kr
- 2Division of Nephrology, Department of Internal Medicine, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 3Organ Transplantation Center, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 4Department of General Surgery, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 5Catholic Hematopoietic Stem Cell Transplantation Center, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- KMID: 2157930
- DOI: http://doi.org/10.3346/jkms.2012.27.7.814
Abstract
- In general, a 2-yr disease-free duration is recommended before kidney transplantation (KT) in end-stage renal disease (ESRD) patients who also have acute leukemia. However, the optimal disease-free interval has not been specified for all subtypes of acute leukemia. Among these subtypes, acute promyelocytic leukemia (APL) shows a favorable prognosis and low relapse rate compared to other types of leukemia. We here report KT after complete remission (CR) of APL in an ESRD patient. Irreversible kidney injury developed in a 23-yr-old man with APL. First, we induced CR and subsequently performed KT 7 months after the achievement of CR. The patient's clinical course after KT was favorable, without allograft rejection or relapse of APL up to1 yr after KT. On the basis of our clinical experience, it is suggested that a long wait may not be necessary before KT in patients with ESRD and APL.
MeSH Terms
-
Adult
Antineoplastic Agents/therapeutic use
Arsenicals/therapeutic use
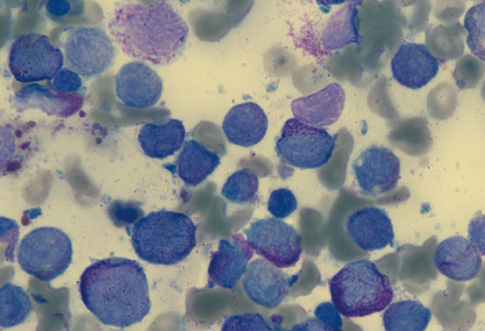
Bone Marrow Cells/pathology
Humans
Kidney Failure, Chronic/*therapy/ultrasonography
*Kidney Transplantation
Leukemia, Promyelocytic, Acute/*diagnosis/drug therapy
Male
Oxides/therapeutic use
Receptors, Retinoic Acid/genetics/metabolism
Remission Induction
Antineoplastic Agents
Arsenicals
Oxides
Receptors, Retinoic Acid
Figure
Reference
-
1. Brenner BM, Rector FC. Brenner and Rector's the kidney. 2004. 7th ed. Philadelphia: Saunders;2.2. Collins AJ, Kasiske B, Herzog C, Chavers B, Foley R, Gilbertson D, Grimm R, Liu J, Louis T, Manning W, et al. Excerpts from the United States Renal Data System 2004 annual data report: atlas of end-stage renal disease in the United States. Am J Kidney Dis. 2005. 45:A5–A7. S1–S280.3. Rama I, Grinyó JM. Malignancy after renal transplantation: the role of immunosuppression. Nat Rev Nephrol. 2010. 6:511–519.4. Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, Rush DN, Vazquez MA, Weir MR. American Society of Transplantation. The evaluation of renal transplantation candidate: clinical practice guideline. Am J Transplant. 2001. 1:3–95.5. Kasiske BL, Snyder JJ, Gilbertson DT, Wang C. Cancer after kidney transplantation in the United States. Am J Transplant. 2004. 4:905–913.6. Sayegh MH, Fine NA, Smith JL, Rennke HG, Milford EL, Tilney NL. Immunologic tolerance to renal allografts after bone marrow transplants from the same donors. Ann Intern Med. 1991. 114:954–955.7. Helg C, Chapuis B, Bolle JF, Morel P, Salomon D, Roux E, Antonioli V, Jeannet M, Leski M. Renal transplantation without immunosuppression in a host with tolerance induced by allogeneic bone marrow transplantation. Transplantation. 1994. 58:1420–1422.8. EBPG (European Expert Group on Renal Transplantation). European Renal Association (ERA-EDTA). European Society for Organ Transplantation (ESOT). European Best Practice Guideline for Renal Transplantation (part 1). Nephrol Dial Transplant. 2000. 15:1–85.9. National Comprehensive Cancer Network ® (NCCN®). NCCN Guidelines version 2. 2011 Acute myeloid leukemia. 2011. 53.10. Niscola P, Vischini G, Tendas A, Scaramucci L, Giovannini M, Bondanini F, Romani C, Brunetti GA, Cartoni C, Cupelli L, et al. Management of hematological malignancies in patients affected by renal failure. Expert Rev Anticancer Ther. 2011. 11:415–432.11. Vesole DH, Jagannath S. Transplants from the same donor. Ann Intern Med. 1992. 116:269–270.12. Gajewski JL, Ippoliti C, Ma Y, Champlin R. Discontinuation of immunosuppression for prevention of kidney graft rejection after receiving a bone marrow transplant from the same HLA identical sibling donor. Am J Hematol. 2002. 71:311–313.13. Hoffman R, Furie B, Benz EJ Jr, McGlave P, Silberstein LE, Shattil SJ. Hematology: basic principles and practice. 2008. 5th ed. Philadelphia: Churchill Livingstone.14. Soignet SL, Peter G. Wintrobe's clinical hematology. 2009. 12th ed. Philadelphia: Lippincott Williams & Wilkins.15. Sanz MA, Lo Coco F, Martin G, Avvisati G, Rayón C, Barbui T, Díaz-Mediavilla J, Fioritoni G, González JD, Liso V, et al. Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups. Blood. 2000. 96:1247–1253.16. Specchia G, Storlazzi CT, Cuneo A, Surace C, Mestice A, Pannunzio A, Rocchi M, Liso V. Acute promyelocytic leukemia with additional chromosome abnormalities in a renal transplant case. Ann Hematol. 2001. 80:246–250.17. Lai CP, Chang CC, Chung CY, Chen ML. Unusual acute promyelocytic leukemia following de novo renal transplant: case report and literature review. Clin Nephrol. 2011. 75:27–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transient spontaneous remission in acute promyelocytic leukemia: two case reports
- Low-dose All-trans Retinoic Acid for Remission Induction of Acute Promyelocytic Leukemia in Acute Renal Failure
- Salvage treatments with all-trans retinoic acid and arsenic trioxide-based regimens in acute promyelocytic leukemia
- A Case of Wernicke Disease in a Patient with Acute Promyelocytic Leukemia
- Remission Induction by Arsenic Trioxide in Patient with Relapsed Acute Promyelocytic Leukemia after Allogeneic Bone Marrow Transplantation