J Korean Med Sci.
2005 Dec;20(6):1082-1084. 10.3346/jkms.2005.20.6.1082.
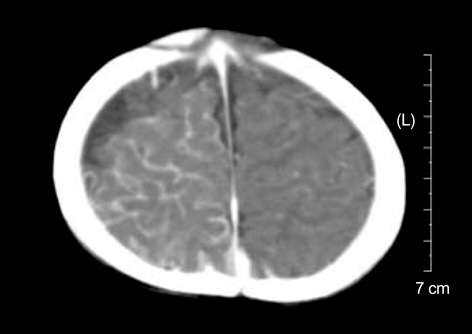
An Infantile Case of Sturge-Weber Syndrome in Association with Klippel-Trenaunay-Weber Syndrome and Phakomatosis Pigmentovascularis
- Affiliations
-
- 1Department of Pediatrics, Wonkwang University School of Medicine, Iksan, Korea. chan33@wonkwang.ac.kr
- KMID: 2157769
- DOI: http://doi.org/10.3346/jkms.2005.20.6.1082
Abstract
- Sturge-Weber syndrome can be associated with facial port-wine stains and intracranial calcification, and concurrent Klippel-Trenaunay-Weber syndrome has been reported. Klippel-Trenaunay-Weber syndrome is a rare congenital mesodermal phakomatosis characterized by cutaneous hemangiomas, venous varicosities and soft tissue or bone hypertrophy of the affected extremities. This report is presented a rare case of the Sturge-Weber syndrome in combination with the Klippel-Trennaunay syndrome and phakomatosis pigmentovascularis in a 4-month-old infant. He showed nevus flameus on the right leg and both part of the face and back, leptomeningeal angiomatosis on right hemisphere, hypertrophy of the right leg, hemiconvulsion on the left and also evidences of congenital glaucoma and nevus of Ota. Very rare case combined with these three kinds of phakomatosis has been reported.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Features and Surgical Outcomes of Sturge-Weber Syndrome with Glaucoma
Jae Hwi Park, Su Ho Lim, Soon Cheol Cha
J Korean Ophthalmol Soc. 2013;54(11):1737-1747. doi: 10.3341/jkos.2013.54.11.1737.
Reference
-
1. Sturge WA. A case of partial epilepsy apparently due to a lesion of one of the vasomotor centers of the brain. Trans Clin Soc Lond. 1879. 12:162–167.2. Barek L, Ledor S, Ledor K. The Klippel-Trenaunay syndrome: a case report and review of the literature. Mt Sinai J Med. 1982. 49:66–70.3. Deutsch J, Weissenbacher G, Widhalm K, Wolf G, Barsegar B. Combination of the syndrome of the Sturge-Weber and the syndrome of Klippel-Trenaunay. Klin Pediatr. 1976. 188:464–471.4. Willliams DW III, Elster AD. Cranial CT and MR in the Klippel-Trenaunay-Weber syndrome. Am J Neuroradiol. 1992. 13:291–294.5. Stephan MJ, Hall BD, Smith DW, Cohen MM. Macrocephaly in association with unusual cutaneous angiomatosis. J Pediatr. 1975. 87:353–359.
Article6. Jaksch H, Bewermeyer H, Dreesbach HA, Heiss WD. Cerebral hemorrhage in arteriovenous malformation associated with Klippel-Trenaunay syndrome. J Neurol. 1986. 233:48–50.7. Boltshauser E, Wilson J, Hoare RD. Sturge-Weber syndrome with bilateral intracranial calcification. J Neurol Neurosurg Psychiatry. 1976. 39:429–435.
Article8. Revol M, Gilly R, Challamel MJ. Epilepsie et maladie de Sturge-Weber. Boll Lega Ital Epil. 1984. 45:51–58.9. Brenner RP, Sharbrough FW. Electroencephalographic evaluation in Sturge-Weber syndrome. Neurology. 1976. 26:629–632.
Article10. Sassower K, Duchowny M, Jayakar P. EEG evaluation in children with Sturge-Weber syndrome and epilepsy. J Epilepsy. 1944. 7:285–289.11. Ogunmekan AO, Hwang PA, Hoffman HJ. Sturge-Weber-Dimitri disease: role of hemispherectomy in prognosis. Can J Neurol Sci. 1989. 16:78–80.12. Ota M. Nevus fusco-caeruleus ophthalmo-maxillaris. Jpn J Dermatol. 1939. 46:369–374.13. Shin SS, Kim SJ, Lee SC, Won YH. A case of phakomatosis pigmentovascularis type IIb associated with perirenal lipomatosis. Korean J Dermatol. 1999. 37:1069–1073.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Phakomatosis Pigmentovascularis Associated with Pyogenic Granuloma as well as Sturge-Weber Syndrome and Klippel-Trenaunay Syndrome
- A Case of Phakomatosis Pigmentovascularis Type IIb Associated with Perirenal Lipomatosis
- A Case of Klippel-Trenaunay Syndrome Combinded with Sturge-Weber Syndrome
- Klippel-trenaunay-weber syndrome
- A Case of Klippel-Trenaunay-Weber Syndrome Diagnosed by Antenatal Ultrasonography