Ann Dermatol.
2015 Dec;27(6):759-762. 10.5021/ad.2015.27.6.759.
Cutaneous and Systemic Plasmacytosis Associated with Renal Amyloidosis
- Affiliations
-
- 1Department of Dermatology, Maryknoll Medical Center, Busan, Korea. heartthrob80@naver.com
- 2Department of Nephrology, Maryknoll Medical Center, Busan, Korea.
- 3Department of Dermatology, Severance Hospital & Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2157456
- DOI: http://doi.org/10.5021/ad.2015.27.6.759
Abstract
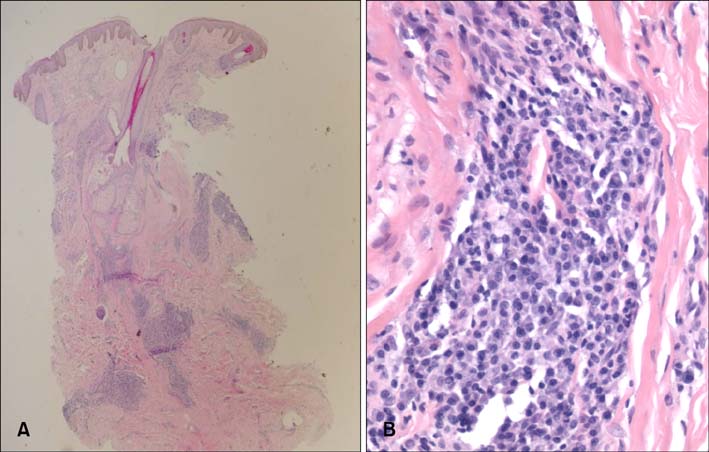
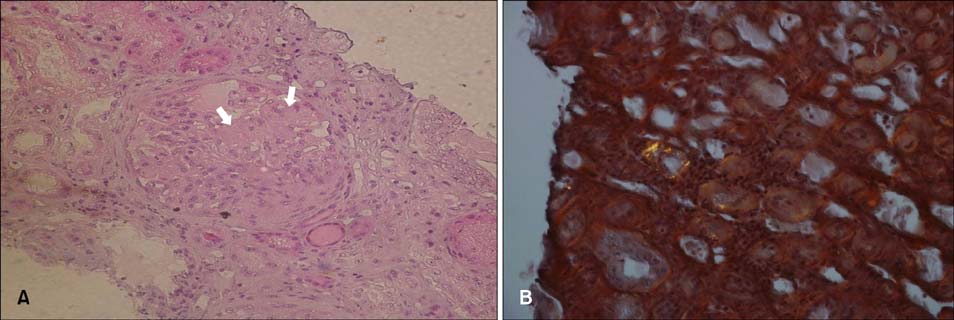
- Cutaneous and systemic plasmacytosis (CSP) is a rare disorder of unknown etiology characterized by cutaneous polyclonal plasma cell infiltrates associated with various extracutaneous involvement and polyclonal hypergammaglobulinemia. Here, we report on a 54-year-old male patient with chronic renal insufficiency who presented with disseminated reddish-brown macules and plaques on the face and trunk. In our evaluation, he was found to have lymphadenopathy, polyclonal hypergammaglobulinemia; benign plasma cell infiltration involving the skin, bone marrow, and retroperitoneal area; and renal amyloidosis. To the best of our knowledge, this is the first reported case of CSP associated with renal amyloidosis.
MeSH Terms
Figure
Reference
-
1. Yashiro A. A kind of plasmacytosis: primary cutaneous plasmacytoma? Jpn J Dermatol. 1976; 86:910.2. Kitamura K, Tamura N, Hatano H, Toyama K, Mikata A, Watanabe S. A case of plasmacytosis with multiple peculiar eruptions. J Dermatol. 1980; 7:341–349.
Article3. Tada Y, Komine M, Suzuki S, Kikuchi K, Sasaki M, Kaneko N, et al. Plasmacytosis: systemic or cutaneous, are they distinct? Acta Derm Venereol. 2000; 80:233–235.
Article4. Ma HJ, Liu W, Li Y, Zhao G, Meng RS, Li DG. Cutaneous and systemic plasmacytosis: a Chinese case. J Dermatol. 2008; 35:536–540.
Article5. Honda R, Cerroni L, Tanikawa A, Ebihara T, Amagai M, Ishiko A. Cutaneous plasmacytosis: report of 6 cases with or without systemic involvement. J Am Acad Dermatol. 2013; 68:978–985.
Article6. Kodama A, Tani M, Hori K, Tozuka T, Matsui T, Ito M, et al. Systemic and cutaneous plasmacytosis with multiple skin lesions and polyclonal hypergammaglobulinaemia: significant serum interleukin-6 levels. Br J Dermatol. 1992; 127:49–53.
Article7. Yamamoto T, Katayama I, Nishioka K. Increased plasma interleukin-6 in cutaneous plasmacytoma: the effect of intralesional steroid therapy. Br J Dermatol. 1997; 137:631–636.
Article8. Lee JS, Chiam L, Tan KB, Salto-Tellez M, Tan SH, Ong BH, et al. Extensive hyperpigmented plaques in a chinese singaporean woman: a case of cutaneous plasmacytosis. Am J Dermatopathol. 2011; 33:498–503.
Article9. Amin HM, McLaughlin P, Rutherford CJ, Abruzzo LV, Jones D. Cutaneous and systemic plasmacytosis in a patient of Asian descent living in the United States. Am J Dermatopathol. 2002; 24:241–245.
Article10. Paydas S. Report on 59 patients with renal amyloidosis. Int Urol Nephrol. 1999; 31:619–631.11. Chen H, Xue Y, Jiang Y, Zeng X, Sun JF. Cutaneous and systemic plasmacytosis showing histopathologic features as mixed-type Castleman disease: a case report. Am J Dermatopathol. 2012; 34:553–556.
Article