Ann Dermatol.
2011 Oct;23(Suppl 2):S274-S278. 10.5021/ad.2011.23.S2.S274.
The Appearance of a Candidate Site for a Primary Melanoma: A 5 Year-gap with a Melanoma of an Unknown Site
- Affiliations
-
- 1Department of Dermatology, Graduate School of Medicine, Chungnam National University, Daejeon, Korea. resina20@cnuh.co.kr
- 2Department of Internal Medicine, Graduate School of Medicine, Chungnam National University, Daejeon, Korea.
- 3Department of Plastic Surgery, Graduate School of Medicine, Chungnam National University, Daejeon, Korea.
- KMID: 2156809
- DOI: http://doi.org/10.5021/ad.2011.23.S2.S274
Abstract
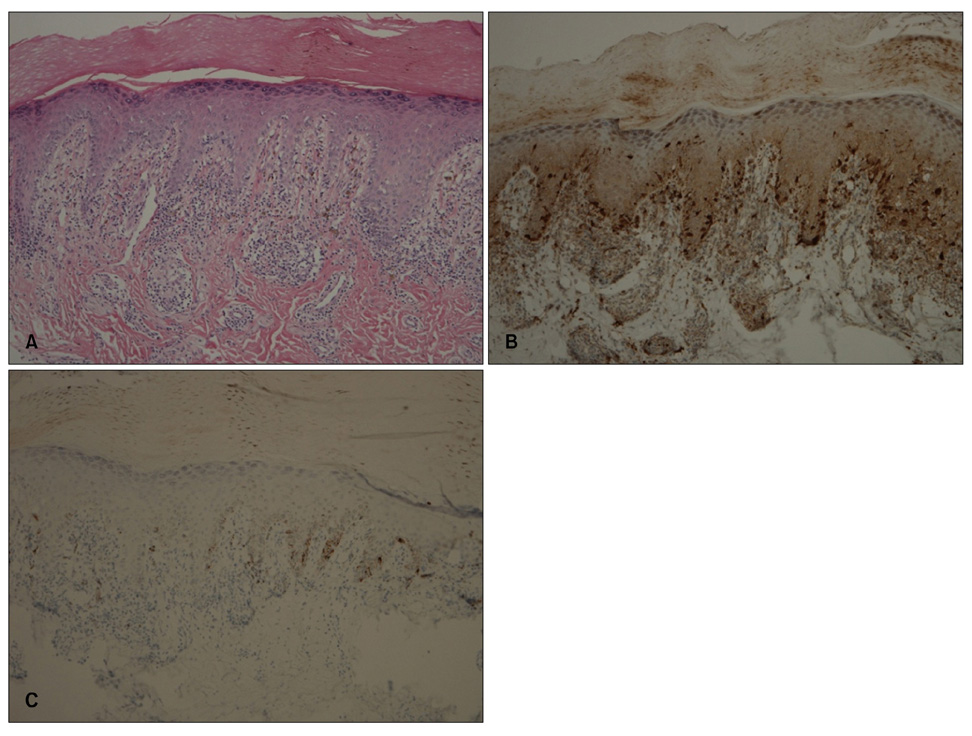
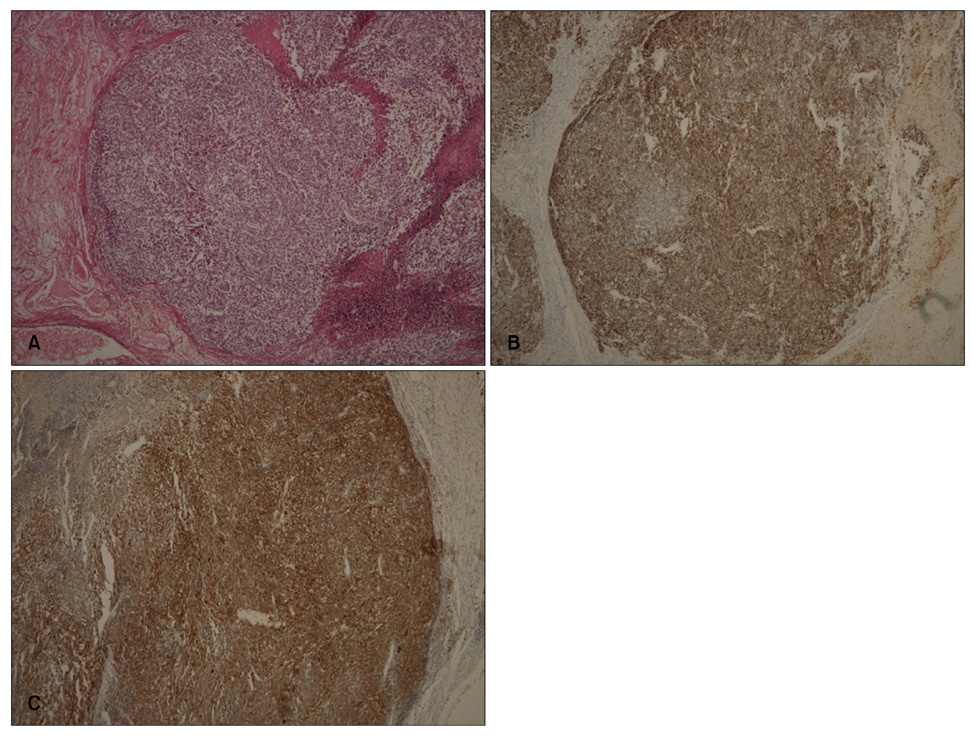
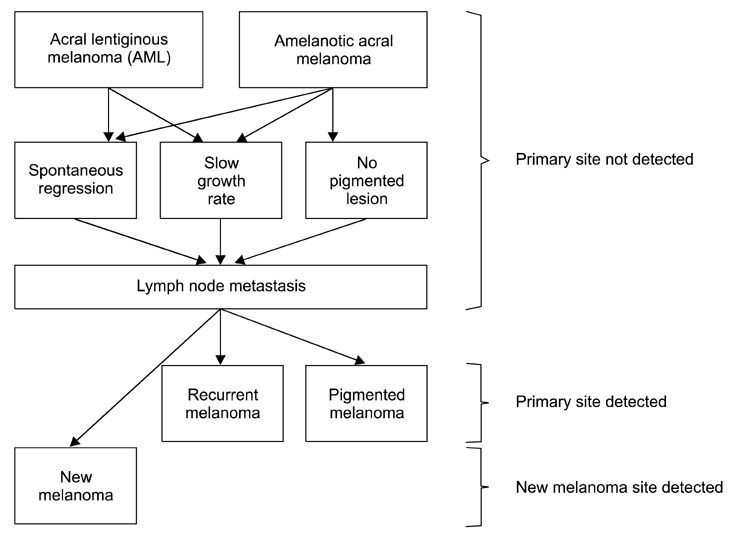
- Although more than 90% of melanomas have cutaneous origins, melanomas sometimes present metastatically with no apparent primary lesion. A 62-year-old female presented with black pigmentation on her left thumbnail that had begun 2 years earlier and after the biopsy, she was diagnosed with malignant melanoma. Interestingly, 7 years earlier, a 4 cm palpable mass on her left axilla had been diagnosed as melanoma from an unknown primary site (MUP) with the involvement of an axillary lymph node. We speculate that the melanoma of the left thumb was the primary site and the melanoma in the axilla was a metastasis from the left thumb, and suggest several hypotheses explaining the appearance of the primary lesion as acral lentiginous melanoma after detecting a metastatic site. We consider this case interesting because it helps us to understand the pathogenesis of MUP and reminds physicians to conduct careful periodical work-ups of melanoma patients, and highlights the importance of continued long-term follow-up, especially for patients with MUP.
MeSH Terms
Figure
Reference
-
1. Anbari KK, Schuchter LM, Bucky LP, Mick R, Synnestvedt M, Guerry D 4th, et al. Melanoma of unknown primary site: presentation, treatment, and prognosis--a single institution study. University of Pennsylvania Pigmented Lesion Study Group. Cancer. 1997. 79:1816–1821.2. Ceballos PI, Barnhill RL. Spontaneous regression of cutaneous tumors. Adv Dermatol. 1993. 8:229–261.3. Blessing K, McLaren KM. Histological regression in primary cutaneous melanoma: recognition, prevalence and significance. Histopathology. 1992. 20:315–322.
Article4. Mahrle C, Bolling R, Gartmann H. Verrucous malignant melanoma (spontaneous regression and simultaneous development of a secondary tumor). Z Hautkr. 1977. 52:897–905.5. Lipsker D, Engel F, Cribier B, Velten M, Hedelin G. Trends in melanoma epidemiology suggest three different types of melanoma. Br J Dermatol. 2007. 157:338–343.
Article6. Kwon IH, Lee JH, Cho KH. Acral lentiginous melanoma in situ: a study of nine cases. Am J Dermatopathol. 2004. 26:285–289.
Article7. Cohen-Solal KA, Crespo-Carbone SM, Namkoong J, Mackason KR, Roberts KG, Reuhl KR, et al. Progressive appearance of pigmentation in amelanotic melanoma lesions. Pigment Cell Res. 2002. 15:282–289.
Article8. Su WP. Malignant melanoma: basic approach to clinicopathologic correlation. Mayo Clin Proc. 1997. 72:267–272.
Article9. Rogers GS, Braun SM. Prognostic factors. Dermatol Clin. 2002. 20:647–658.
Article10. Zettersten E, Shaikh L, Ramirez R, Kashani-Sabet M. Prognostic factors in primary cutaneous melanoma. Surg Clin North Am. 2003. 83:61–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Malignant Melanoma with Nodal Metastasis from Unknown Primary Site
- Unknow Primary Melanoma
- A Case of Metastatic Endobronchial Melanoma from an Unknown Primary Site
- Malignant Melanoma of Unknown Primary Origin Presenting as Cardiac Metastasis
- Four Cases of Primary Malignant Melanoma of the Nasal Cavity