J Korean Neurosurg Soc.
2015 Dec;58(6):518-527. 10.3340/jkns.2015.58.6.518.
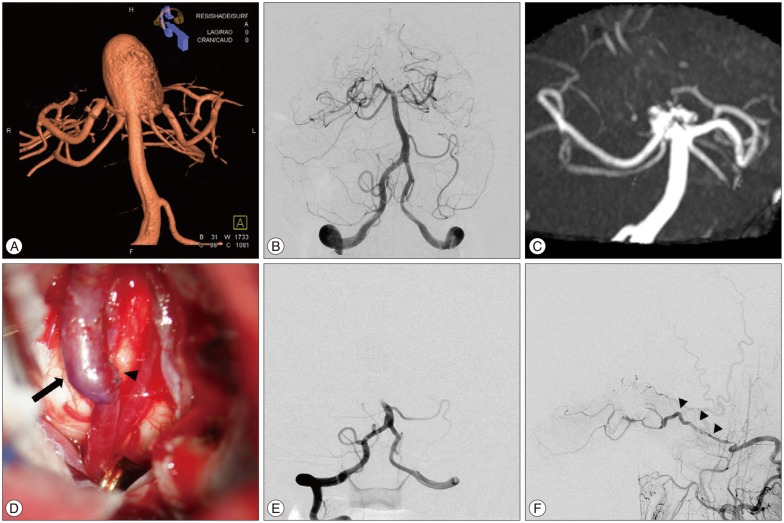
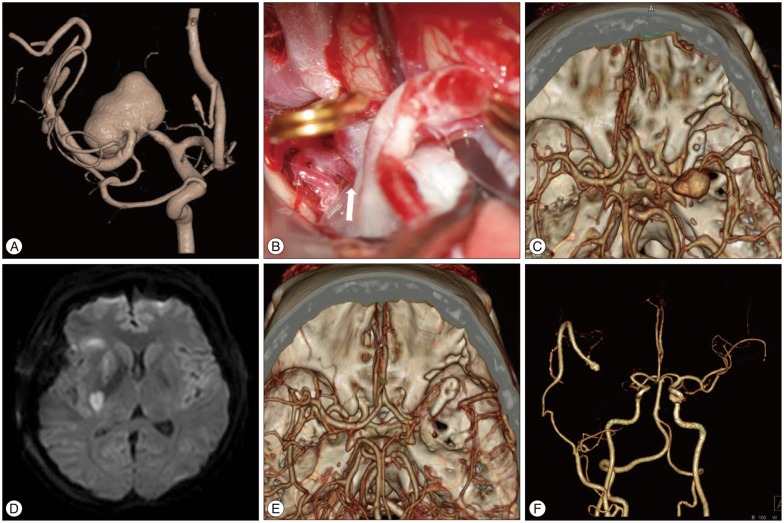
Surgical Flow Alteration for the Treatment of Intracranial Aneurysms That Are Unclippable, Untrappable, and Uncoilable
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jsahn@amc.seoul.kr
- 2Department of Neurosurgery, College of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2151153
- DOI: http://doi.org/10.3340/jkns.2015.58.6.518
Abstract
OBJECTIVE
The treatment of complex intracranial aneurysms remains challenging. One approach is the application of surgical flow alteration to treat aneurysms that are neither clippable, trappable, or coilable. The efficacy and limitations of surgical flow alteration have not yet been established.
METHODS
Cases of complex aneurysms treated with surgical flow alteration (proximal occlusion with or without bypass, distal occlusion with or without bypass and bypass only) were included in this retrospective study.
RESULTS
Among a total of 16 cases, there were 7 giant aneurysms (> or =25 mm diameter) and 9 large aneurysms (>10 mm diameter); 15 of 16 aneurysms were unruptured. There were 8 aneurysms located in the anterior circulation, while the other 8 were in the posterior circulation. Aneurysms were treated with proximal occlusion in 10 cases and distal occlusion in 5 cases; in 1 case, the aneurysm occluded spontaneously after bypass without parent artery occlusion. All but 2 cases underwent prior or concurrent bypass surgery. Complete obliteration of the aneurysm at the latest imaging follow-up was shown in 12 of 16 cases (75.0%). Bypass patency was confirmed in 13 of 15 cases (86.7%). Surgery-related morbidity developed in 3 cases (18.8%, Glasgow outcome scale of 4) and all were perforator infarctions. There were no mortalities.
CONCLUSION
Surgical flow alteration resulted in a high rate of aneurysmal obliteration with acceptable morbidity. Although several limitations remained, it could represent an alternative method for treating complex aneurysms.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Outcomes of Large (>10 mm) Unruptured Posterior Circulation Aneurysms and Their Predictors
Joonho Byun, Wonhyoung Park, Jung Cheol Park, Jae Sung Ahn
J Korean Neurosurg Soc. 2021;64(1):39-50. doi: 10.3340/jkns.2020.0028.
Reference
-
1. Aymard A, Hodes JE, Rüfenacht D, Merland JJ. Endovascular treatment of a giant fusiform aneurysm of the entire basilar artery. AJNR Am J Neuroradiol. 1992; 13:1143–1146. PMID: 1636527.2. Barrow DL, Spetzler RF. Cotton-clipping technique to repair intraoperative aneurysm neck tear : a technical note. Neurosurgery. 2011; 68(2):Suppl Operative. 294–299. discussion 299PMID: 21368700.3. Bederson JB, Spetzler RF. Anastomosis of the anterior temporal artery to a secondary trunk of the middle cerebral artery for treatment of a giant M1 segment aneurysm. Case report. J Neurosurg. 1992; 76:863–866. PMID: 1564547.
Article4. Bederson JB, Zabramski JM, Spetzler RF. Treatment of fusiform intracranial aneurysms by circumferential wrapping with clip reinforcement. Technical note. J Neurosurg. 1992; 77:478–480. PMID: 1506900.
Article5. Benashvili GM, Alexander LF, Zubkov YN. Thrombosis of a giant aneurysm after extracranial-intracranial bypass. Neurosurgery. 1992; 31:360–364. PMID: 1513444.
Article6. Ceylan S, Karakuş A, Duru S, Baykal S, Ilbay K. Reconstruction of the middle cerebral artery after excision of a giant fusiform aneurysm. Neurosurg Rev. 1998; 21:189–193. PMID: 9795960.
Article7. Choudhari KA. Wrapping and coating of cerebral aneurysms : history, evolution and surgical management after a re-bleed. Br J Neurosurg. 2004; 18:259–267. PMID: 15327228.
Article8. Deshmukh VR, Kakarla UK, Figueiredo EG, Zabramski JM, Spetzler RF. Long-term clinical and angiographic follow-up of unclippable wrapped intracranial aneurysms. Neurosurgery. 2006; 58:434–442. discussion 434-442PMID: 16528182.
Article9. Dolenc V. Direct microsurgical repair of intracavernous vascular lesions. J Neurosurg. 1983; 58:824–831. PMID: 6854374.
Article10. Drake CG, Peerless SJ. Giant fusiform intracranial aneurysms : review of 120 patients treated surgically from 1965 to 1992. J Neurosurg. 1997; 87:141–162. PMID: 9254076.
Article11. Drake CG, Peerless SJ, Ferguson GG. Hunterian proximal arterial occlusion for giant aneurysms of the carotid circulation. J Neurosurg. 1994; 81:656–665. PMID: 7931611.
Article12. Fujitsu K, Ishiwata Y, Gondo G, Fujii S, Feng DD. Wrap-clipping with a Dacron mesh silastic sheet. Technical note. J Neurosurg. 1994; 80:336–337. PMID: 8283276.13. Gobin YP, Counord JL, Flaud P, Duffaux J. In vitro study of haemodynamics in a giant saccular aneurysm model : influence of flow dynamics in the parent vessel and effects of coil embolisation. Neuroradiology. 1994; 36:530–536. PMID: 7845578.
Article14. Haque R, Kellner C, Solomon RA. Spontaneous thrombosis of a giant fusiform aneurysm following extracranial-intracranial bypass surgery. J Neurosurg. 2009; 110:469–474. PMID: 19012486.
Article15. Hoh BL, Putman CM, Budzik RF, Carter BS, Ogilvy CS. Combined surgical and endovascular techniques of flow alteration to treat fusiform and complex wide-necked intracranial aneurysms that are unsuitable for clipping or coil embolization. J Neurosurg. 2001; 95:24–35. PMID: 11453395.
Article16. Horowitz MB, Yonas H, Jungreis C, Hung TK. Management of a giant middle cerebral artery fusiform serpentine aneurysm with distal clip application and retrograde thrombosis : case report and review of the literature. Surg Neurol. 1994; 41:221–225. PMID: 8146737.
Article17. Iplikcioglu AC, Dinc C, Bek S, Bikmaz K. Spontaneous thrombosis and resorption of a giant fusiform A2 aneurysm. Case illustration. J Neurosurg. 2006; 105:788. PMID: 17121148.18. Isla A, Alvarez F, Roda JM, Muñoz J, Morales C, Garcia Blazquez M. Serpentine aneurysm : regrowth after a superficial temporal artery-middle cerebral artery bypass and internal carotid artery ligation : case report. Neurosurgery. 1994; 34:1072–1074. PMID: 8084393.
Article19. Kalani MY, Zabramski JM, Hu YC, Spetzler RF. Extracranial-intracranial bypass and vessel occlusion for the treatment of unclippable giant middle cerebral artery aneurysms. Neurosurgery. 2013; 72:428–435. discussion 435-436PMID: 23208054.
Article20. Lawton MT, Hamilton MG, Morcos JJ, Spetzler RF. Revascularization and aneurysm surgery : current techniques, indications, and outcome. Neurosurgery. 1996; 38:83–92. discussion 92-94PMID: 8747955.21. Lawton MT, Spetzler RF. Surgical strategies for giant intracranial aneurysms. Neurosurg Clin N Am. 1998; 9:725–742. PMID: 9738103.
Article22. Lee KC, Joo JY, Lee KS, Shin YS. Recanalization of completely thrombosed giant aneurysm : case report. Surg Neurol. 1999; 51:94–98. PMID: 9952130.23. Lee SJ, Ahn JS, Kwun BD, Kim CJ. Giant serpentine aneurysm of the middle cerebral artery. J Korean Neurosurg Soc. 2010; 48:177–180. PMID: 20856671.
Article24. Lee SY, Sekhar LN. Treatment of aneurysms by excision or trapping with arterial reimplantation or interpositional grafting. Report of three cases. J Neurosurg. 1996; 85:178–185. PMID: 8683271.
Article25. Mahadevan A, Tagore R, Siddappa NB, Santosh V, Yasha TC, Ranga U, et al. Giant serpentine aneurysm of vertebrobasilar artery mimicking dolichoectasia--an unusual complication of pediatric AIDS. Report of a case with review of the literature. Clin Neuropathol. 2008; 27:37–52. PMID: 18257473.
Article26. Mai JC, Tariq F, Kim LJ, Sekhar LN. Flow diversion radial artery bypass graft coupled with terminal basilar artery occlusion for the treatment of complex basilar apex aneurysms : operative nuances. Neurosurgery. 2013; 72(2):Suppl Operative. ons116–ons126. discussion ons126PMID: 23313975.27. Mathis JM, Barr JD, Jungreis CA, Yonas H, Sekhar LN, Vincent D, et al. Temporary balloon test occlusion of the internal carotid artery : experience in 500 cases. AJNR Am J Neuroradiol. 1995; 16:749–754. PMID: 7611033.28. Miyamoto S, Funaki T, Iihara K, Takahashi JC. Successful obliteration and shrinkage of giant partially thrombosed basilar artery aneurysms through a tailored flow reduction strategy with bypass surgery. J Neurosurg. 2011; 114:1028–1036. PMID: 20932097.
Article29. Nussbaum ES, Madison MT, Goddard JK, Lassig JP, Janjua TM, Nussbaum LA. Remote distal outflow occlusion : a novel treatment option for complex dissecting aneurysms of the posterior inferior cerebellar artery. Report of 3 cases. J Neurosurg. 2009; 111:78–83. PMID: 19301964.
Article30. Quiñones-Hinojosa A, Lawton MT. In situ bypass in the management of complex intracranial aneurysms : technique application in 13 patients. Neurosurgery. 2005; 57(1):Suppl. 140–145. discussion 140-145PMID: 15987580.
Article31. Sanai N, Zador Z, Lawton MT. Bypass surgery for complex brain aneurysms : an assessment of intracranial-intracranial bypass. Neurosurgery. 2009; 65:670–683. discussion 683PMID: 19834371.32. Sari A, Kandemir S, Kuzeyli K, Dinc H. Giant serpentine aneurysm with acute spontaneous complete thrombosis. AJNR Am J Neuroradiol. 2006; 27:766–768. PMID: 16611761.33. Scott RM, Liu HC, Yuan R, Adelman L. Rupture of a previously unruptured giant middle cerebral artery aneurysm after extracranial-intracranial bypass surgery. Neurosurgery. 1982; 10:600–603. PMID: 7099411.
Article34. Shojima M, Morita A, Kimura T, Oshima M, Kin T, Saito N. Computational fluid dynamic simulation of a giant basilar tip aneurysm with eventual rupture after Hunterian ligation. World Neurosurg. 2014; 82:535.e5–535.e9. PMID: 24067739.
Article35. Steinberg GK, Drake CG, Peerless SJ. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms. Immediate results and long-term outcome in 201 patients. J Neurosurg. 1993; 79:161–173. PMID: 8331396.
Article36. Suzuki S, Takahashi T, Ohkuma H, Shimizu T, Fujita S. Management of giant serpentine aneurysms of the middle cerebral artery--review of literature and report of a case successfully treated by STA-MCA anastomosis only. Acta Neurochir (Wien). 1992; 117:23–29. PMID: 1514425.
Article37. Takahashi JC, Murao K, Iihara K, Nonaka Y, Taki J, Nagata I, et al. Successful "blind-alley" formation with bypass surgery for a partially thrombosed giant basilar artery tip aneurysm refractory to upper basilar artery obliteration. Case report. J Neurosurg. 2007; 106:484–487. PMID: 17367074.
Article38. Yang K, Ahn JS, Park JC, Kwon do H, Kwun BD, Kim CJ. The efficacy of bypass surgery using a short interposition graft for the treatment of intracranial complex aneurysm. World Neurosurg. 2015; 83:197–202. PMID: 24933242.
Article39. Yasui T, Komiyama M, Iwai Y, Yamanaka K, Matsusaka Y, Morikawa T, et al. Regrowth and fatal rerupture despite proximal occlusion after coil embolization of a ruptured large basilar bifurcation aneurysm--case report. Neurol Med Chir (Tokyo). 2004; 44:587–590. PMID: 15686178.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Bypass Surgery for Treating Unclippable and Uncoilable Aneurysms
- Circumferential Wrapping and Clipping with Temporalis Fascia for Treatment of Unclippable Intracranial Aneurysms
- Revascularization in the Management of Complex Cerebral Aneurysm
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms
- Guideline for Management of Unruptured Intracranial Aneurysms: Preliminary Report