Hip Pelvis.
2015 Dec;27(4):258-264. 10.5371/hp.2015.27.4.258.
Does the Time of Postoperative Bisphosphonate Administration Affect the Bone Union in Osteoporotic Intertrochanteric Fracture of Femur?
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyung Hee University School of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea. khrhyu@gmail.com
- 3Department of Orthopedic Surgery, Inha University College of Medicine, Incheon, Korea.
- KMID: 2150514
- DOI: http://doi.org/10.5371/hp.2015.27.4.258
Abstract
- PURPOSE
This study was designed to investigate the effect of bisphosphonate administration starting time on bone healing and to identify the best administration time following surgical treatment of osteoporotic intertrochanteric fractures.
MATERIALS AND METHODS
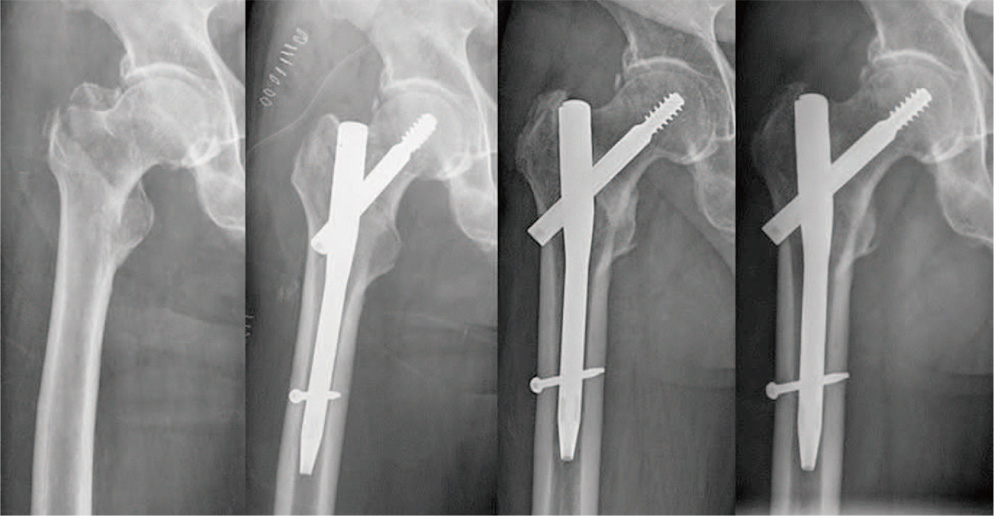
Two hundreds and eighty four patients (284 hips; 52 males, 232 females) who underwent surgery following osteoporotic intertrochanteric fracture from December 2002 to December 2012 were retrospectively analyzed. The average follow-up period was 68.4 months. The patients were divided into three groups according to the time of bisphosphonate administration after operation: 1 week (group A; n=102), 1 month (group B; n=89), and 3 months (group C; n=93). Koval scores and change of Koval scores 1 year after operation were used for clinical evaluation. For radiologic evaluation, the time of callus appearance across the fracture line on sagittal and coronal radiographs and the time to absence of pain during hip motion was judged as the time of bone union.
RESULTS
Koval scores one year after surgery for groups A, B, and C were 2.44, 2.36, and 2.43 (P=0.895), respectively. The mean time of union was 12.4, 11.9, and 12.3 weeks after operation in the three groups (P=0.883), respectively. There were zero cases of nonunion. There were 3, 5, and 7 cases of fixative displacement in the three groups, respectively, but the distribution showed no significant difference (P>0.472).
CONCLUSION
The initiating time of bisphosphonate administration following surgery does not affect the clinical outcomes in patients with osteoporotic intertrochanteric fracture.
MeSH Terms
Figure
Cited by 1 articles
-
Effect of Preoperative Bisphosphonate Treatment on Fracture Healing after Internal Fixation Treatment of Intertrochanteric Femoral Fractures
Eic Ju Lim, Jung-Taek Kim, Chul-Ho Kim, Ji Wan Kim, Jae Suk Chang, Pil Whan Yoon
Hip Pelvis. 2019;31(2):75-81. doi: 10.5371/hp.2019.31.2.75.
Reference
-
1. Murakami H, Takahashi N, Sasaki T, et al. A possible mechanism of the specific action of bisphosphonates on osteoclasts: tiludronate preferentially affects polarized osteoclasts having ruffled borders. Bone. 1995; 17:137–144.
Article2. Sato M, Grasser W. Effects of bisphosphonates on isolated rat osteoclasts as examined by reflected light microscopy. J Bone Miner Res. 1990; 5:31–40.
Article3. Bartl R. Update 2004. Osteoporosis--management--current status. Krankenpfl J. 2004; 42:232.4. Shin CS, Choi HJ, Kim MJ, et al. Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone. 2010; 47:378–387.
Article5. Solomon DH, Hochberg MC, Mogun H, Schneeweiss S. The relation between bisphosphonate use and non-union of fractures of the humerus in older adults. Osteoporos Int. 2009; 20:895–901.
Article6. Davidson CW, Merrilees MJ, Wilkinson TJ, McKie JS, Gilchrist NL. Hip fracture mortality and morbidity--can we do better? N Z Med J. 2001; 114:329–332.7. Lee SR, Kim SR, Chung KH, et al. Mortality and activity after hip fracture: a prospective study. J Korean Orthop Assoc. 2005; 40:423–427.
Article8. Moon ES, Kim HS, Park JO, et al. The incidence of new vertebral compression fractures in women after kyphoplasty and factors involved. Yonsei Med J. 2007; 48:645–652.
Article9. Yoon HK, Cho DY, Shin DE, Song SJ, Kim JH, Yoon BH. Clinical distribution of bilateral non-contemporary hip fractures in elderly patients. J Korean Fract Soc. 2005; 18:375–378.
Article10. Gardner MJ, Flik KR, Mooar P, Lane JM. Improvement in the undertreatment of osteoporosis following hip fracture. J Bone Joint Surg Am. 2002; 84-A:1342–1348.
Article11. Ha YC, Kim SR, Koo KH, et al. An epidemiological study of hip fracture in Jeju island, Korea. J Korean Orthop Assoc. 2004; 39:131–136.
Article12. Yim SJ, Lee YK, Kim CK, Song HS, Kang HK. Results of osteoporotic treatment drug after periarticular fracture of hip. J Korean Fract Soc. 2010; 23:167–171.
Article13. Li J, Mori S, Kaji Y, Mashiba T, Kawanishi J, Norimatsu H. Effect of bisphosphonate (incadronate) on fracture healing of long bones in rats. J Bone Miner Res. 1999; 14:969–979.
Article14. Li C, Mori S, Li J, et al. Long-term effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res. 2001; 16:429–436.
Article15. Bauss F, Schenk RK, Hört S, Müller-Beckmann B, Sponer G. New model for simulation of fracture repair in fullgrown beagle dogs: model characterization and results from a long-term study with ibandronate. J Pharmacol Toxicol Methods. 2004; 50:25–34.
Article16. Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res. 2004; 19:1779–1786.
Article17. Rozental TD, Vazquez MA, Chacko AT, Ayogu N, Bouxsein ML. Comparison of radiographic fracture healing in the distal radius for patients on and off bisphosphonate therapy. J Hand Surg Am. 2009; 34:595–602.
Article18. Amanat N, Brown R, Bilston LE, Little DG. A single systemic dose of pamidronate improves bone mineral content and accelerates restoration of strength in a rat model of fracture repair. J Orthop Res. 2005; 23:1029–1034.
Article19. Goodship AE, Walker PC, McNally D, Chambers T, Green JR. Use of a bisphosphonate (pamidronate) to modulate fracture repair in ovine bone. Ann Oncol. 1994; 5:Suppl 7. S53–S55.20. Little DG, McDonald M, Bransford R, Godfrey CB, Amanat N. Manipulation of the anabolic and catabolic responses with OP-1 and zoledronic acid in a rat critical defect model. J Bone Miner Res. 2005; 20:2044–2052.
Article21. Bransford R, Goergens E, Briody J, Amanat N, Cree A, Little D. Effect of zoledronic acid in an L6-L7 rabbit spine fusion model. Eur Spine J. 2007; 16:557–562.
Article22. Xu XL, Gou WL, Wang AY, et al. Basic research and clinical applications of bisphosphonates in bone disease: what have we learned over the last 40 years? J Transl Med. 2013; 11:303.23. Odvina CV, Levy S, Rao S, Zerwekh JE, Rao DS. Unusual mid-shaft fractures during long-term bisphosphonatetherapy. Clin Endocrinol (Oxf). 2010; 72:161–168.24. Ha YC, Cho MR, Park KH, Kim SY, Koo KH. Is surgery necessary for femoral insufficiency fractures after longterm bisphosphonate therapy? Clin Orthop Relat Res. 2010; 468:3393–3398.
Article25. Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011; 71:186–190.
Article26. Bobyn JD, Hacking SA, Krygier JJ, Harvey EJ, Little DG, Tanzer M. Zoledronic acid causes enhancement of bone growth into porous implants. J Bone Joint Surg Br. 2005; 87:416–420.
Article27. Molvik H, Khan W. Bisphosphonates and their influence on fracture healing: a systematic review. Osteoporos Int. 2015; 26:1251–1260.
Article28. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.
Article29. Gong HS, Song CH, Lee YH, Rhee SH, Lee HJ, Baek GH. Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am. 2012; 94:1729–1736.
Article30. Abrahamsen B, Eiken P, Eastell R. Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res. 2009; 24:1095–1102.
Article31. Harris LJ, Tarr RR. Implant failures in orthopaedic surgery. Biomater Med Devices Artif Organs. 1979; 7:243–255.
Article32. Koval KJ, Zuckerman JD. Hip fractures: II. Evaluation and treatment of intertrochanteric fractures. J Am Acad Orthop Surg. 1994; 2:150–156.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Bone Graft in the Treatment of Osteoporotic Unstable Intertrochanteric Fracture of the Femur
- Clinical features of atypical femur fracture
- Influence of Oral and Intravenous Bisphosphonate for the Patients Treated Surgically in Osteoporotic Distal Radius Fracture
- Insufficiency Fracture of Ipsilateral Femur Neck in Patient Treated with Long Term Bisphosphonate Treatment: A Case Report
- Influence of Early Bisphosphonate Administration for Fracture Healing in Patients with Osteoporotic Proximal Humerus Fractures