J Korean Soc Radiol.
2016 Jan;74(1):15-21. 10.3348/jksr.2016.74.1.15.
Recurrent and Second Breast Cancer Detected on Follow-Up Mammography and Breast Ultrasound after Breast-Conserving Surgery: Imaging Findings and Clinicopathologic Factors
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiology, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea. jhcha@amc.seoul.kr
- KMID: 2150458
- DOI: http://doi.org/10.3348/jksr.2016.74.1.15
Abstract
- PURPOSE
To assess the imaging and clinicopathologic outcomes of recurrent and second breast cancer after breast-conserving surgery for invasive ductal carcinomas detected on follow-up mammography and breast ultrasound (US).
MATERIALS AND METHODS
Seventy-six women with an ipsilateral breast tumor recurrence (IBTR) or regional lymph node recurrence and/or contralateral breast cancer (RLNR & CBC) after breast-conserving surgery were included in this study. The mammography and US images were analyzed and the clinicopathologic parameters were compared between the groups.
RESULTS
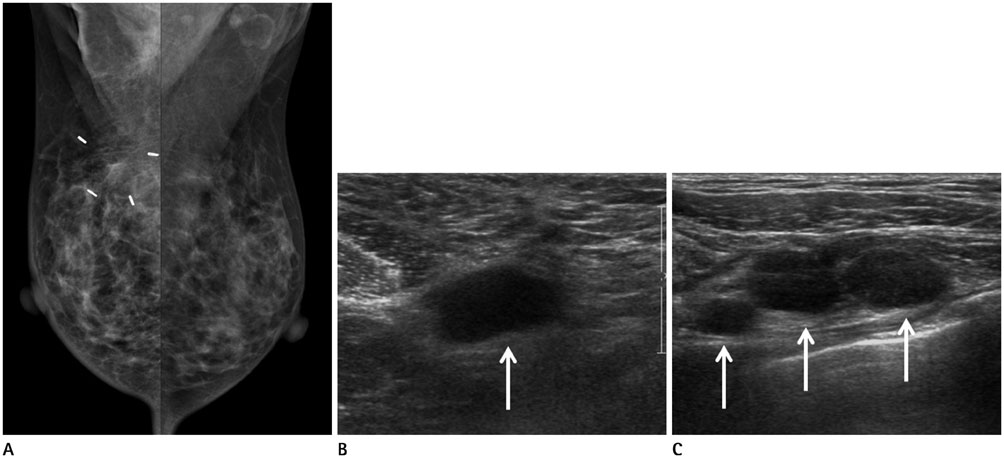
Thirty had an IBTR, and 46 had a RLNR & CBC. The IBTR group's mammography and US images frequently revealed calcification and masses on the breast, respectively. The most frequent site of RLNR detected during follow-up mammography and breast US was the axilla. In univariate analysis, the tumors in the IBTR group were predominantly estrogen receptor (ER)-negative, HER-2 overexpression, and p53-positive. ER and HER-2 were shown by the multivariate analysis to be independent parameters associated for both types of recurrences.
CONCLUSION
A mass or calcification is frequently present in IBTR and the axillary lymph node is the most frequent site of RLNR. ER and HER-2 status are major independent factors associated with recurrent and second breast cancer.
MeSH Terms
Figure
Reference
-
1. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241.2. Jatoi I, Proschan MA. Randomized trials of breast-conserving therapy versus mastectomy for primary breast cancer: a pooled analysis of updated results. Am J Clin Oncol. 2005; 28:289–294.3. Lu WL, Jansen L, Post WJ, Bonnema J, Van de Velde JC, De Bock GH. Impact on survival of early detection of isolated breast recurrences after the primary treatment for breast cancer: a meta-analysis. Breast Cancer Res Treat. 2009; 114:403–412.4. Touboul E, Buffat L, Belkacémi Y, Lefranc JP, Uzan S, Lhuillier P, et al. Local recurrences and distant metastases after breast-conserving surgery and radiation therapy for early breast cancer. Int J Radiat Oncol Biol Phys. 1999; 43:25–38.5. Nixon AJ, Neuberg D, Hayes DF, Gelman R, Connolly JL, Schnitt S, et al. Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. J Clin Oncol. 1994; 12:888–894.6. Kini VR, Vicini FA, Frazier R, Victor SJ, Wimbish K, Martinez AA. Mammographic, pathologic, and treatment-related factors associated with local recurrence in patients with early-stage breast cancer treated with breast conserving therapy. Int J Radiat Oncol Biol Phys. 1999; 43:341–346.7. Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Breast-conserving therapy for macroscopically multiple cancers. Ann Surg. 1990; 212:38–44.8. Recht A, Come SE, Henderson IC, Gelman RS, Silver B, Hayes DF, et al. The sequencing of chemotherapy and radiation therapy after conservative surgery for early-stage breast cancer. N Engl J Med. 1996; 334:1356–1361.9. Veronesi U, Marubini E, Del Vecchio M, Manzari A, Andreola S, Greco M, et al. Local recurrences and distant metastases after conservative breast cancer treatments: partly independent events. J Natl Cancer Inst. 1995; 87:19–27.10. Magee B, Swindell R, Harris M, Banerjee SS. Prognostic factors for breast recurrence after conservative breast surgery and radiotherapy: results from a randomised trial. Radiother Oncol. 1996; 39:223–227.11. Freedman GM, Fowble BL. Local recurrence after mastectomy or breast-conserving surgery and radiation. Oncology (Williston Park). 2000; 14:1561–1581. discussion 1581-1582, 1582-158412. Park CC, Mitsumori M, Nixon A, Recht A, Connolly J, Gelman R, et al. Outcome at 8 years after breast-conserving surgery and radiation therapy for invasive breast cancer: influence of margin status and systemic therapy on local recurrence. J Clin Oncol. 2000; 18:1668–1675.13. Khatcheressian JL, Wolff AC, Smith TJ, Grunfeld E, Muss HB, Vogel VG, et al. American Society of Clinical Oncology 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting. J Clin Oncol. 2006; 24:5091–5097.14. Francis M, Cakir B, Ung O, Gebski V, Boyages J. Prognosis after breast recurrence following conservative surgery and radiotherapy in patients with node-negative breast cancer. Br J Surg. 1999; 86:1556–1562.15. Kim SJ, Moon WK, Cho N, Chang JM. The detection of recurrent breast cancer in patients with a history of breast cancer surgery: comparison of clinical breast examination, mammography and ultrasonography. Acta Radiol. 2011; 52:15–20.16. Shin JH, Han BK, Choe YH, Nam SJ, Park W, Im YH. Ultrasonographic detection of occult cancer in patients after surgical therapy for breast cancer. J Ultrasound Med. 2005; 24:643–649.17. Moon HJ, Kim MJ, Kim EK, Park BW, Youk JH, Kwak JY, et al. US surveillance of regional lymph node recurrence after breast cancer surgery. Radiology. 2009; 252:673–681.18. Komoike Y, Akiyama F, Iino Y, Ikeda T, Akashi-Tanaka S, Ohsumi S, et al. Ipsilateral breast tumor recurrence (IBTR) after breast-conserving treatment for early breast cancer: risk factors and impact on distant metastases. Cancer. 2006; 106:35–41.19. Noguchi S, Koyama H, Kasugai T, Tsukuma H, Tsuji N, Tsuda H, et al. A case-control study on risk factors for local recurrences or distant metastases in breast cancer patients treated with breast-conserving surgery. Oncology. 1997; 54:468–474.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidental Breast Cancers Identified in the One-Stop Symptomatic Breast Clinic
- Usefulness of Ultrasonography for Detection of Breast Cancer in Patients under 30 Years of Age
- Hemangiomas with the Variable Manifestations on Breast Imaging: Three Case Reports
- Incidentally detected insitu ductal carcinoma with mastitis
- Early screening for breast cancer