Korean J Pain.
2015 Jul;28(3):203-209. 10.3344/kjp.2015.28.3.203.
A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea. mhyoon@jnu.ac.kr
- KMID: 2149465
- DOI: http://doi.org/10.3344/kjp.2015.28.3.203
Abstract
- BACKGROUND
Ketorolac has been used as a postoperative analgesia in combination with opioids. However, the use of ketorolac may produce serious side effects in vulnerable patients. Propacetamol is known to induce fewer side effects than ketorolac because it mainly affects the central nervous system. We compared the analgesic effects and patient satisfaction levels of each drug when combined with fentanyl patient-controlled analgesia (PCA).
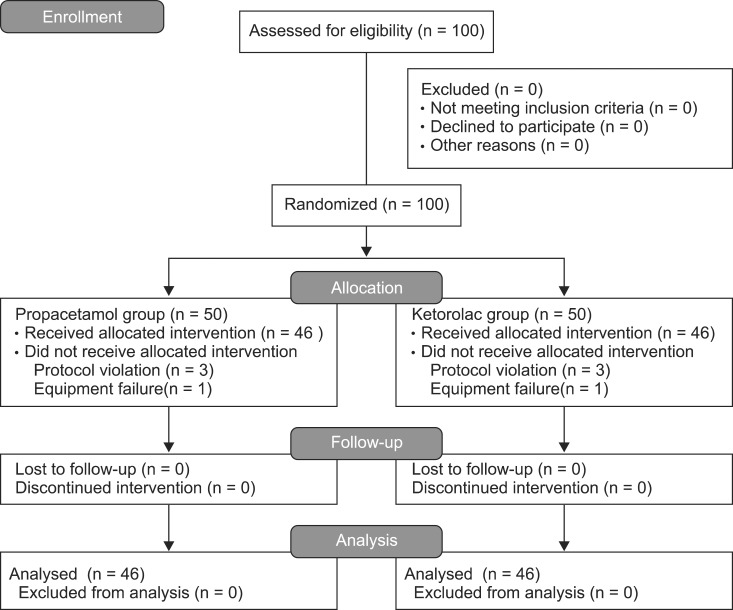
METHODS
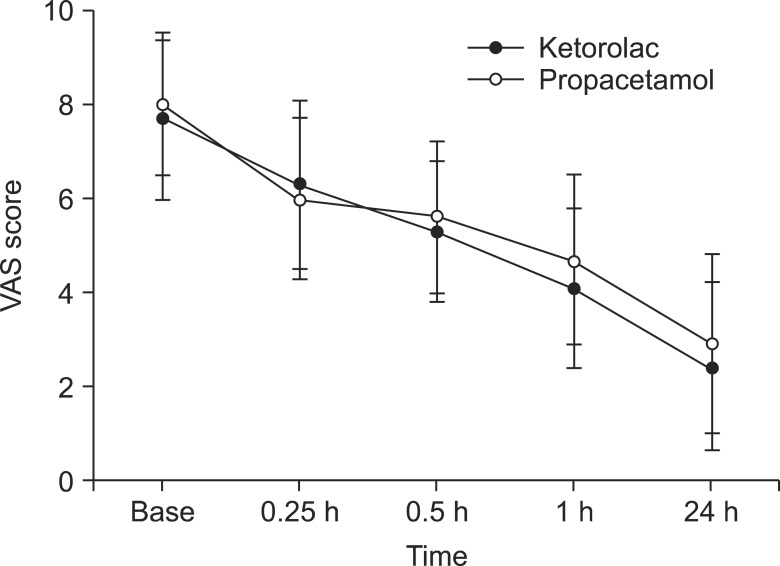
The patients were divided into two groups, each with n = 46. The patients in each group were given 60 mg of ketorolac or 2 g of propacetamol (mixed with fentanyl) for 10 minutes. The patients were then given 180 mg of ketorolac or 8 g of propacetamol (mixed with fentanyl and ramosetron) through PCA. We assessed the visual analogue pain scale (VAS) at the time point immediately before administration (baseline) and at 15, 30, and 60 minutes, and 24 hours after administration. Also, the side effects of each regimen and each patient's degree of satisfaction were assessed.
RESULTS
There was a significant decline in the VAS score in both groups (P < 0.05). However, there were no significant differences in the VAS scores between the groups at each time point. Satisfaction scores between the groups showed no significant difference.
CONCLUSIONS
The efficacy of propacetamol is comparable to that of ketorolac in postoperative PCA with fentanyl.
MeSH Terms
Figure
Reference
-
1. Weis OF, Sriwatanakul K, Alloza JL, Weintraub M, Lasagna L. Attitudes of patients, housestaff, and nurses toward postoperative analgesic care. Anesth Analg. 1983; 62:70–74. PMID: 6129821.
Article2. Melzack R, Abbott FV, Zackon W, Mulder DS, Davis MW. Pain on a surgical ward: a survey of the duration and intensity of pain and the effectiveness of medication. Pain. 1987; 29:67–72. PMID: 3588001.
Article3. Moote C. Efficacy of nonsteroidal anti-inflammatory drugs in the management of postoperative pain. Drugs. 1992; 44(Suppl 5):14–29. PMID: 1284558.
Article4. Dahl JB, Kehlet H. Non-steroidal anti-inflammatory drugs: rationale for use in severe postoperative pain. Br J Anaesth. 1991; 66:703–712. PMID: 2064886.
Article5. Fredman B, Olsfanger D, Jedeikin R. A comparative study of ketorolac and diclofenac on post-laparoscopic cholecystectomy pain. Eur J Anaesthesiol. 1995; 12:501–504. PMID: 8542859.6. O'Hara DA, Fragen RJ, Kinzer M, Pemberton D. Ketorolac tromethamine as compared with morphine sulfate for treatment of postoperative pain. Clin Pharmacol Ther. 1987; 41:556–561. PMID: 3568540.7. Yee JP, Koshiver JE, Allbon C, Brown CR. Comparison of intramuscular ketorolac tromethamine and morphine sulfate for analgesia of pain after major surgery. Pharmacotherapy. 1986; 6:253–261. PMID: 3540877.
Article8. Cashman J, McAnulty G. Nonsteroidal anti-inflammatory drugs in perisurgical pain management. Mechanisms of action and rationale for optimum use. Drugs. 1995; 49:51–70. PMID: 7705216.
Article9. Kenny GN. Potential renal, haematological and allergic adverse effects associated with nonsteroidal anti-inflammatory drugs. Drugs. 1992; 44(Suppl 5):31–36. PMID: 1284559.
Article10. Sachs CJ. Oral analgesics for acute nonspecific pain. Am Fam Physician. 2005; 71:913–918. PMID: 15768621.11. Hyllested M, Jones S, Pedersen JL, Kehlet H. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: a qualitative review. Br J Anaesth. 2002; 88:199–214. PMID: 11878654.
Article12. Graham GG, Scott KF. Mechanism of action of paracetamol. Am J Ther. 2005; 12:46–55. PMID: 15662292.
Article13. Remy C, Marret E, Bonnet F. Effects of acetaminophen on morphine side-effects and consumption after major surgery: meta-analysis of randomized controlled trials. Br J Anaesth. 2005; 94:505–513. PMID: 15681586.
Article14. Björkman R, Hallman KM, Hedner J, Hedner T, Henning M. Acetaminophen blocks spinal hyperalgesia induced by NMDA and substance P. Pain. 1994; 57:259–264. PMID: 7524008.
Article15. Bonnefont J, Courade JP, Alloui A, Eschalier A. Antinociceptive mechanism of action of paracetamol. Drugs. 2003; 63 Spec No 2:1–4. PMID: 14758785.16. Bannwarth B, Netter P, Lapicque F, Gillet P, Péré P, Boccard E, et al. Plasma and cerebrospinal fluid concentrations of paracetamol after a single intravenous dose of propacetamol. Br J Clin Pharmacol. 1992; 34:79–81. PMID: 1633071.
Article17. Evans CJ, Trudeau E, Mertzanis P, Marquis P, Peña BM, Wong J, et al. Development and validation of the Pain Treatment Satisfaction Scale (PTSS): a patient satisfaction questionnaire for use in patients with chronic or acute pain. Pain. 2004; 112:254–266. PMID: 15561380.
Article18. Zhou TJ, Tang J, White PF. Propacetamol versus ketorolac for treatment of acute postoperative pain after total hip or knee replacement. Anesth Analg. 2001; 92:1569–1575. PMID: 11375848.
Article19. McQuay HJ, Poppleton P, Carroll D, Summerfield RJ, Bullingham RE, Moore RA. Ketorolac and acetaminophen for orthopedic postoperative pain. Clin Pharmacol Ther. 1986; 39:89–93. PMID: 3510797.
Article20. Varrassi G, Marinangeli F, Agrò F, Aloe L, De Cillis P, De Nicola A, et al. A double-blinded evaluation of propacetamol versus ketorolac in combination with patient-controlled analgesia morphine: analgesic efficacy and tolerability after gynecologic surgery. Anesth Analg. 1999; 88:611–616. PMID: 10072016.
Article21. Mayes S, Ferrone M. Fentanyl HCl patient-controlled iontophoretic transdermal system for the management of acute postoperative pain. Ann Pharmacother. 2006; 40:2178–2186. PMID: 17164395.
Article22. Kollender Y, Bickels J, Stocki D, Maruoani N, Chazan S, Nirkin A, et al. Subanaesthetic ketamine spares postoperative morphine and controls pain better than standard morphine does alone in orthopaedic-oncological patients. Eur J Cancer. 2008; 44:954–962. PMID: 18396035.
Article23. Mao J, Price DD, Mayer DJ. Mechanisms of hyperalgesia and morphine tolerance: a current view of their possible interactions. Pain. 1995; 62:259–274. PMID: 8657426.
Article24. Tveita T, Thoner J, Klepstad P, Dale O, Jystad A, Borchgrevink PC. A controlled comparison between single doses of intravenous and intramuscular morphine with respect to analgesic effects and patient safety. Acta Anaesthesiol Scand. 2008; 52:920–925. PMID: 18702754.
Article25. Parker RK, Holtmann B, Smith I, White PF. Use of ketorolac after lower abdominal surgery. Effect on analgesic requirement and surgical outcome. Anesthesiology. 1994; 80:6–12. PMID: 8291731.
Article26. Sevarino FB, Sinatra RS, Paige D, Ning T, Brull SJ, Silverman DG. The efficacy of intramuscular ketorolac in combination with intravenous PCA morphine for postoperative pain relief. J Clin Anesth. 1992; 4:285–288. PMID: 1419009.
Article27. Rogers JE, Fleming BG, Macintosh KC, Johnston B, Morgan-Hughes JO. Effect of timing of ketorolac administration on patient-controlled opioid use. Br J Anaesth. 1995; 75:15–18. PMID: 7669460.
Article28. Ready LB, Brown CR, Stahlgren LH, Egan KJ, Ross B, Wild L, et al. Evaluation of intravenous ketorolac administered by bolus or infusion for treatment of postoperative pain. A double-blind, placebo-controlled, multicenter study. Anesthesiology. 1994; 80:1277–1286. PMID: 8010474.
Article29. Gillis JC, Brogden RN. Ketorolac. A reappraisal of its pharmacodynamic and pharmacokinetic properties and therapeutic use in pain management. Drugs. 1997; 53:139–188. PMID: 9010653.30. Koh SC, Pua HL, Tay DH, Ratnam SS. The effects of gynaecological surgery on coagulation activation, fibrinolysis and fibrinolytic inhibitor in patients with and without ketorolac infusion. Thromb Res. 1995; 79:501–514. PMID: 7502276.
Article31. Varrassi G, Panella L, Piroli A, Marinangeli F, Varrassi S, Wolman I, et al. The effects of perioperative ketorolac infusion on postoperative pain and endocrine-metabolic response. Anesth Analg. 1994; 78:514–519. PMID: 8109770.
Article32. Strom BL, Berlin JA, Kinman JL, Spitz PW, Hennessy S, Feldman H, et al. Parenteral ketorolac and risk of gastrointestinal and operative site bleeding. A postmarketing surveillance study. JAMA. 1996; 275:376–382. PMID: 8569017.
Article33. Henry D, Lim LL, Garcia Rodriguez LA, Perez Gutthann S, Carson JL, Griffin M, et al. Variability in risk of gastrointestinal complications with individual non-steroidal anti-inflammatory drugs: results of a collaborative meta-analysis. BMJ. 1996; 312:1563–1566. PMID: 8664664.
Article34. García Rodríguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual nonsteroidal anti-inflammatory drugs. Lancet. 1994; 343:769–772. PMID: 7907735.
Article35. Cummings DM, Amadio P Jr. A review of selected newer nonsteroidal anti-inflammatory drugs. Am Fam Physician. 1994; 49:1197–1202. PMID: 8154406.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of ketorolac and propacetamol on pain control after tonsillectomy in pediatric patients
- Propacetamol as an alternative of ketorolac for postoperative pain management using patient-controlled analgesia
- The Analgesic Efficacy of Transdermal Fentanyl Patch with Intravenous Ketorolac by Patient Controlled Analgesia after Total Abdominal Hysterectomy
- A Effectiveness of Butorphanol and Nalbuphine as Utilized with Ketorolac in Patient Controlled Analgesia after Total Abdominal Hysterectomy
- The Morphine-Sparing Effect of Propacetamol on Patient Controlled Analgesia in Gynecological Surgery