Cancer Res Treat.
2015 Jul;47(3):473-479. 10.4143/crt.2014.115.
Body Mass Index and Doses at Organs at Risk in a Mediterranean Population Treated with Postoperative Vaginal Cuff Brachytherapy
- Affiliations
-
- 1Department of Radiation Oncology, Complejo Hospitalario Universitario de Albacete, Albacete, Spain. ssabaterm@gmail.com
- 2Department of Radiation Oncology, Hospital Universitari Sant Joan, Reus, Spain.
- 3Department of Radiation Oncology, Hospital Son Espases, Palma de Mallorca, Spain.
- 4Department of Radiation Oncology, Hospital Central, Oviedo, Spain.
- 5Gynecological Cancer Unit, Radiation Oncology Department, ICMHO, Hospital Clinic, University of Barcelona, IDIBAPS, Barcelona, Spain.
- KMID: 2148497
- DOI: http://doi.org/10.4143/crt.2014.115
Abstract
- PURPOSE
Association between body mass index (BMI) and doses in organs at risk during postoperative vaginal cuff brachytherapy (VCB) treatment has not been evaluated. The aim of this study was to analyse the impact of BMI on the dose delivered to bladder and rectum during high-dose-rate VCB using computed tomography (CT) scans at every fraction.
MATERIALS AND METHODS
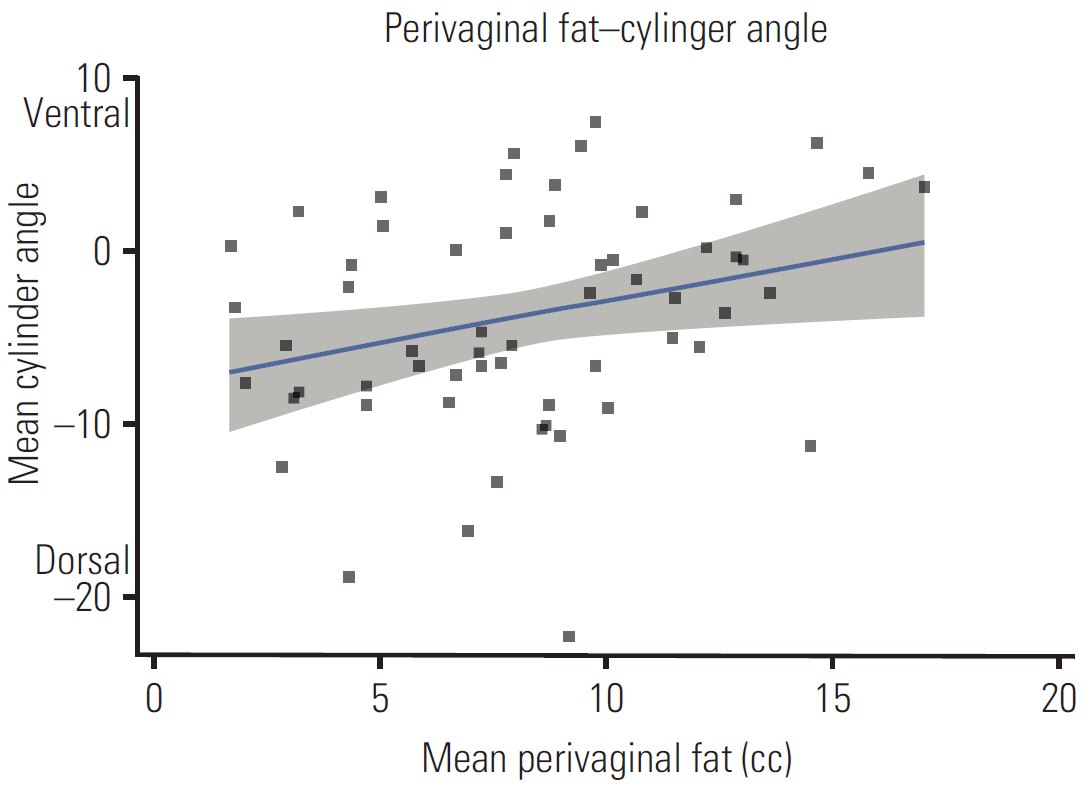
A retrospective analysis of 220 planning CT sets derived from 59 patients was conducted. Every planning CT was re-segmented and re-planned under the same parameters. Rectum and bladder dose-volume histogram values (D0.1cc, D1cc, and D2cc) were extracted and evaluated. The mean values for all applications per patient were calculated and correlated with BMI, as well as other factors influencing rectal and bladder doses. Multiple regression analysis performed to model organ at risk dose-volume parameters.
RESULTS
According to World Health Organization (WHO), 6.8% of patients were normal, 35.6% were overweight, and 57.6% were class I obese. Median rectal doses were 133.5%, 110.9%, and 99.3% for D(0.1cc), D(1cc), and D(2cc), respectively. The corresponding median bladder doses were 96.2%, 80.6%, and 73.3%, respectively. BMI did not show significant association with rectal doses. However, BMI did show a significant association with evaluated bladder dose metrics (D(0.1cc), r=-0.366, p=0.004; D(1cc), r=-0.454, p < 0.001; D2cc, r=-0.451, p < 0.001). BMI was retained in the multivariate regression models (D(0.1cc), p=0.004; D(1cc), p < 0.001; D(2cc), p=0.001).
CONCLUSION
In this group of Mediterranean, overweight, and moderately obese patients, BMI showed association with lower bladder dose values, but not with rectal doses.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Fader AN, Arriba LN, Frasure HE, von Gruenigen VE. Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol. 2009; 114:121–7.
Article2. Arem H, Park Y, Pelser C, Ballard-Barbash R, Irwin ML, Hollenbeck A, et al. Prediagnosis body mass index, physical activity, and mortality in endometrial cancer patients. J Natl Cancer Inst. 2013; 105:342–9.
Article3. van Roermund JG, Hinnen KA, Tolman CJ, Bol GH, Witjes JA, Bosch JL, et al. Periprostatic fat correlates with tumour aggressiveness in prostate cancer patients. BJU Int. 2011; 107:1775–9.
Article4. Patil N, Crook J, Saibishkumar EP, Aneja M, Borg J, Pond G, et al. The effect of obesity on rectal dosimetry after permanent prostate brachytherapy. Brachytherapy. 2009; 8:218–22.
Article5. Boyle JM, Craciunescu O, Steffey B, Cai J, Chino J. Body mass index, dose to organs at risk during vaginal brachytherapy, and the role of three-dimensional CT-based treatment planning. Brachytherapy. 2014; 13:332–6.
Article6. Jia WP, Lu JX, Xiang KS, Bao YQ, Lu HJ, Chen L. Prediction of abdominal visceral obesity from body mass index, waist circumference and waist-hip ratio in Chinese adults: receiver operating characteristic curves analysis. Biomed Environ Sci. 2003; 16:206–11.7. Lear SA, Humphries KH, Kohli S, Birmingham CL. The use of BMI and waist circumference as surrogates of body fat differs by ethnicity. Obesity (Silver Spring). 2007; 15:2817–24.
Article8. Rapp K, Schroeder J, Klenk J, Stoehr S, Ulmer H, Concin H, et al. Obesity and incidence of cancer: a large cohort study of over 145,000 adults in Austria. Br J Cancer. 2005; 93:1062–7.
Article9. Reeves KW, Carter GC, Rodabough RJ, Lane D, McNeeley SG, Stefanick ML, et al. Obesity in relation to endometrial cancer risk and disease characteristics in the Women's Health Initiative. Gynecol Oncol. 2011; 121:376–82.
Article10. Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995; 333:677–85.
Article11. Arem H, Chlebowski R, Stefanick ML, Anderson G, Wactawski-Wende J, Sims S, et al. Body mass index, physical activity, and survival after endometrial cancer diagnosis: results from the Women's Health Initiative. Gynecol Oncol. 2013; 128:181–6.
Article12. von Gruenigen VE, Tian C, Frasure H, Waggoner S, Keys H, Barakat RR. Treatment effects, disease recurrence, and survival in obese women with early endometrial carcinoma: a Gynecologic Oncology Group study. Cancer. 2006; 107:2786–91.13. Crosbie EJ, Roberts C, Qian W, Swart AM, Kitchener HC, Renehan AG. Body mass index does not influence post-treatment survival in early stage endometrial cancer: results from the MRC ASTEC trial. Eur J Cancer. 2012; 48:853–64.
Article14. Arem H, Irwin ML. Obesity and endometrial cancer survival: a systematic review. Int J Obes (Lond). 2013; 37:634–9.
Article15. Nout RA, Smit VT, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomised trial. Lancet. 2010; 375:816–23.
Article16. Sabater S, Andres I, Sevillano M, Berenguer R, Machin-Hamalainen S, Arenas M. Dose accumulation during vaginal cuff brachytherapy based on rigid/deformable registration vs. single plan addition. Brachytherapy. 2014; 13:343–51.
Article17. Sabater S, Sevillano MM, Andres I, Berenguer R, Machin-Hamalainen S, Muller K, et al. Reduction of rectal doses by removal of gas in the rectum during vaginal cuff brachytherapy. Strahlenther Onkol. 2013; 189:951–6.
Article18. Hoskin PJ, Bownes P, Summers A. The influence of applicator angle on dosimetry in vaginal vault brachytherapy. Br J Radiol. 2002; 75:234–7.
Article19. Hung J, Shen S, De Los Santos JF, Kim RY. Image-based 3D treatment planning for vaginal cylinder brachytherapy: dosimetric effects of bladder filling on organs at risk. Int J Radiat Oncol Biol Phys. 2012; 83:980–5.
Article20. Sabater S, Andres A, de la Vara Olivas V, Sevillano M, Berenguer R, Carrizo MV, et al. Effect of rectal distention on vaginal cuff brachytherapy. Radiother Oncol. 2013; 106:s365–6.21. Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004; 4:579–91.
Article22. Small W Jr, Beriwal S, Demanes DJ, Dusenbery KE, Eifel P, Erickson B, et al. American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. Brachytherapy. 2012; 11:58–67.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on Repairing Method of Vaginal Cuff in Total Laparoscopic Hysterectomy
- Design of a New Applicator for High-Dose Rate Vaginal Brachytherapy
- A comparative Study for morbidity and Compilication in Total AbdominalHysterectomy ; -Open Versus Closed Vaginal Cuff
- Radiation Dose Calculation in the Surrounding Organs during Brachytherapy of Prostate Cancer
- Impact of vaginal cylinder diameter on outcomes following brachytherapy for early stage endometrial cancer