Cancer Res Treat.
2015 Jul;47(3):436-440. 10.4143/crt.2013.184.
Potential Role of Adjuvant Radiation Therapy in Cervical Thymic Neoplasm Involving Thyroid Gland or Neck
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2148492
- DOI: http://doi.org/10.4143/crt.2013.184
Abstract
- PURPOSE
The purpose of this study is to assess the clinicopathologic features, treatment outcomes, and role of adjuvant radiation therapy (RT) in cervical thymic neoplasm involving the thyroid gland or neck.
MATERIALS AND METHODS
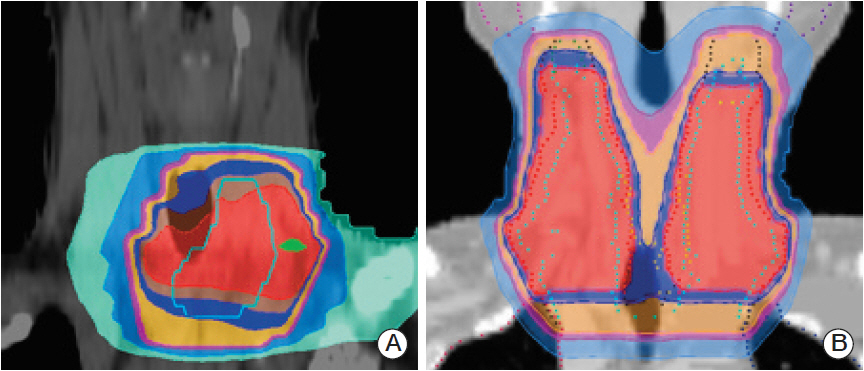
The medical and pathologic records of eight patients with cervical thymic neoplasm were reviewed retrospectively. All patients underwent surgical resection, including thyroidectomy or mass excision. Adjuvant RT was added in five patients with adverse clinicopathologic features. The radiation doses ranged from 54 Gy/27 fractions to 66 Gy/30 fractions delivered to the primary tumor bed and pathologically involved regional lymphatics using a 3-dimensional conformal technique.
RESULTS
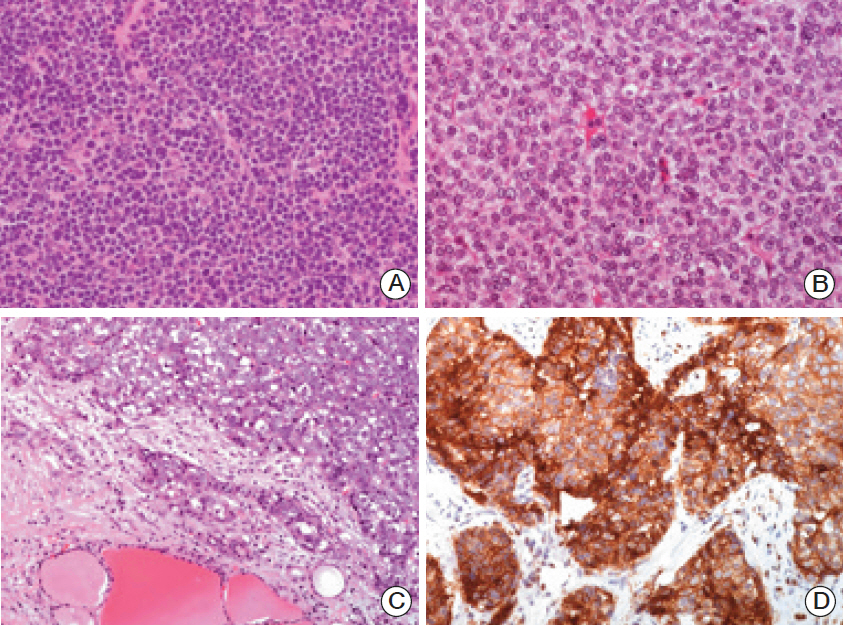
Eight cases of cervical thymic neoplasm included three patients with carcinoma showing thymus-like differentiation (CASTLE) and five with ectopic cervical thymoma. The histologic subtypes of ectopic cervical thymoma patients were World Health Organization (WHO) type B3 thymoma in one, WHO type B1 thymoma in two, WHO type AB thymoma in one, and metaplastic thymoma in one, respectively. The median age was 57 years (range, 40 to 76 years). Five patients received adjuvant RT: three with CASTLE; one with WHO type B3; and one with WHO type AB with local invasiveness. After a median follow-up period of 49 months (range, 11 to 203 months), no recurrence had been observed, regardless of adjuvant RT.
CONCLUSION
Adjuvant RT after surgical resection might be worthwhile in patients with CASTLE and ectopic cervical thymoma with WHO type B2-C and/or extraparenchymal extension, as similarly indicated for primary thymic epithelial tumors. A longer follow-up period may be needed in order to validate this strategy.
MeSH Terms
Figure
Reference
-
References
1. Wu TH, Jin JS, Huang TW, Chang H, Lee SC. Ectopic cervical thymoma in a patient with myasthenia gravis. J Cardiothorac Surg. 2011; 6:89.
Article2. Oh YL, Ko YH, Ree HJ. Aspiration cytology of ectopic cervical thymoma mimicking a thyroid mass: a case report. Acta Cytol. 1998; 42:1167–71.3. Hsu IL, Wu MH, Lai WW, Lin MY, Chang JM, Yen YT, et al. Cervical ectopic thymoma. J Thorac Cardiovasc Surg. 2007; 133:1658–9.
Article4. Taweevisit M, Sampatanukul P, Thorner PS. Ectopic thymoma can mimic benign and malignant thyroid lesions on fine needle aspiration cytology: a case report and literature review. Acta Cytol. 2013; 57:213–20.
Article5. Miyauchi A, Kuma K, Matsuzuka F, Matsubayashi S, Kobayashi A, Tamai H, et al. Intrathyroidal epithelial thymoma: an entity distinct from squamous cell carcinoma of the thyroid. World J Surg. 1985; 9:128–35.
Article6. Chan JK, Rosai J. Tumors of the neck showing thymic or related branchial pouch differentiation: a unifying concept. Hum Pathol. 1991; 22:349–67.
Article7. Roka S, Kornek G, Schuller J, Ortmann E, Feichtinger J, Armbruster C. Carcinoma showing thymic-like elements: a rare malignancy of the thyroid gland. Br J Surg. 2004; 91:142.8. Reimann JD, Dorfman DM, Nose V. Carcinoma showing thymus-like differentiation of the thyroid (CASTLE): a comparative study: evidence of thymic differentiation and solid cell nest origin. Am J Surg Pathol. 2006; 30:994–1001.9. Ito Y, Miyauchi A, Nakamura Y, Miya A, Kobayashi K, Kakudo K. Clinicopathologic significance of intrathyroidal epithelial thymoma/carcinoma showing thymus-like differentiation: a collaborative study with Member Institutes of The Japanese Society of Thyroid Surgery. Am J Clin Pathol. 2007; 127:230–6.10. DeLellis RA, Lloyd RV, Heitz PU, Eng C. World Health Organization classification of tumors: pathology and genetics of tumours of endocrine organs. 3rd ed. Lyon: IARC Press;2004.11. Sun T, Wang Z, Wang J, Wu Y, Li D, Ying H. Outcome of radical resection and postoperative radiotherapy for thyroid carcinoma showing thymus-like differentiation. World J Surg. 2011; 35:1840–6.
Article12. Luo CM, Hsueh C, Chen TM. Extrathyroid carcinoma showing thymus-like differentiation (CASTLE) tumor: a new case report and review of literature. Head Neck. 2005; 27:927–33.13. Chow SM, Chan JK, Tse LL, Tang DL, Ho CM, Law SC. Carcinoma showing thymus-like element (CASTLE) of thyroid: combined modality treatment in 3 patients with locally advanced disease. Eur J Surg Oncol. 2007; 33:83–5.
Article14. Oh D, Ahn YC, Kim K, Kim J, Shim YM, Han J. Is there a role of postoperative radiation therapy in completely resected stage I/II thymic epithelial tumor? Cancer Res Treat. 2012; 44:166–72.
Article15. Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC. Pathology and genetics of tumours of the lung, pleura, thymus and heart. Lyon: IARC Press;2004.16. Kang G, Yoon N, Han J, Kim YE, Kim TS, Kim K. Metaplastic thymoma: report of 4 cases. Korean J Pathol. 2012; 46:92–5.
Article17. Dorfman DM, Shahsafaei A, Miyauchi A. Intrathyroidal epithelial thymoma (ITET)/carcinoma showing thymus-like differentiation (CASTLE) exhibits CD5 immunoreactivity: new evidence for thymic differentiation. Histopathology. 1998; 32:104–9.
Article18. Chang S, Joo M, Kim H. Cytologic findings of thyroid carcinoma showing thymus-like differentiation: a case report. Korean J Pathol. 2012; 46:302–5.
Article19. Youens KE, Bean SM, Dodd LG, Jones CK. Thyroid carcinoma showing thymus-like differentiation (CASTLE): case report with cytomorphology and review of the literature. Diagn Cytopathol. 2011; 39:204–9.
Article20. Chang ST, Chuang SS. Ectopic cervical thymoma: a mimic of T-lymphoblastic lymphoma. Pathol Res Pract. 2003; 199:633–5.
Article21. Masaoka A, Monden Y, Nakahara K, Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer. 1981; 48:2485–92.
Article22. Chen YD, Feng QF, Lu HZ, Mao YS, Zhou ZM, Ou GF, et al. Role of adjuvant radiotherapy for stage II thymoma after complete tumor resection. Int J Radiat Oncol Biol Phys. 2010; 78:1400–6.
Article23. Chang JH, Kim HJ, Wu HG, Kim JH, Kim YT. Postoperative radiotherapy for completely resected stage II or III thymoma. J Thorac Oncol. 2011; 6:1282–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Ectopic Cervical Thymic Tumors Mimicking as Thyroid Tumors
- Ectopic cervical thymic squamous cell carcinoma misdiagnosed as thyroid cancer: a case report
- Postoperative Radiotherapy in Thymic Carcinoma : A case report
- A Case of Ectopic Lateral Cervical Thymic Cyst Mimicking as a Second Branchial Cleft Cyst
- Fibrosarcoma of the Thyroid Gland : Report of a Case