Ann Rehabil Med.
2015 Aug;39(4):645-648. 10.5535/arm.2015.39.4.645.
Myotonic Dystrophy Type 1 Complicated With Peripheral Arterial Occlusive Disease: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. skyler02@hallym.or.kr
- KMID: 2148238
- DOI: http://doi.org/10.5535/arm.2015.39.4.645
Abstract
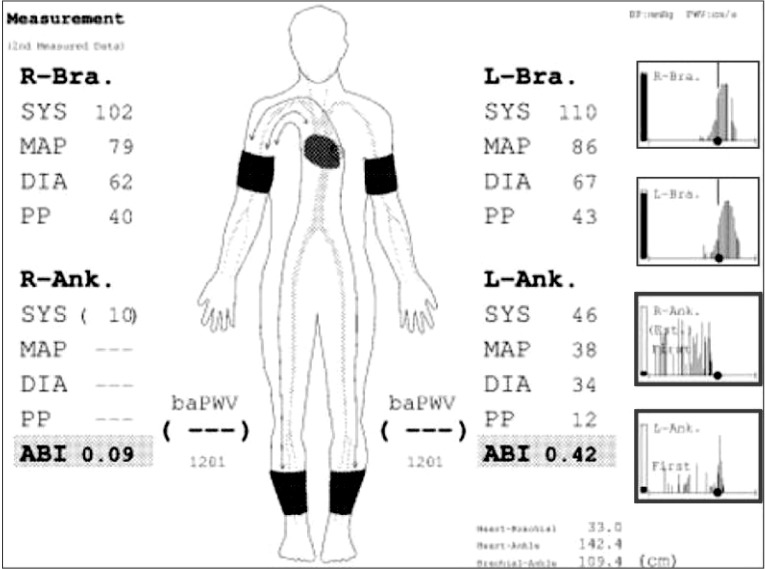
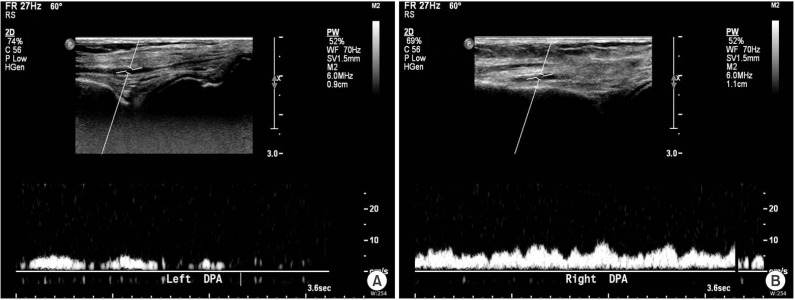
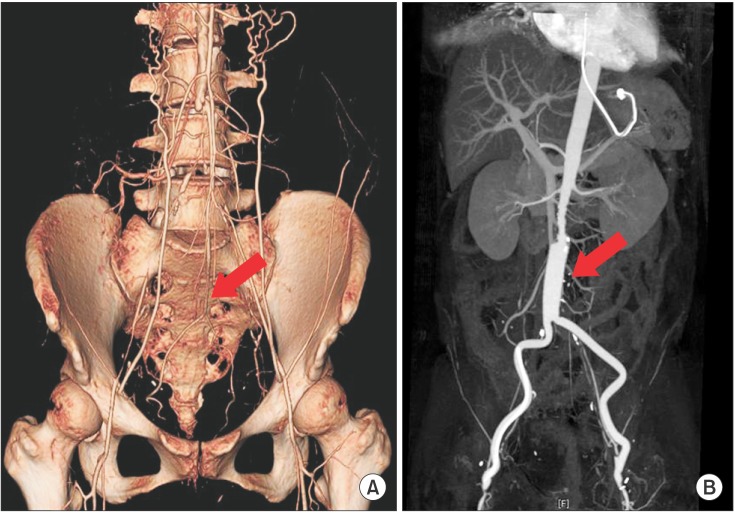
- Myotonic dystrophy (MD) is the most common adult muscular dystrophy characterized by multi-systemic clinical manifestations involving the brain, smooth muscle, cardiovascular and endocrine systems. However, peripheral arterial occlusive disease (PAOD) is an uncommon presentation of MD type 1 (DM1), which has not been reported in recent literature. A 53-year-old female, previously confirmed as DM1, presented with vague claudication of both lower limbs. The diagnosis of PAOD based on results of ankle-brachial index, ultrasonography, and abdominal computed tomography angiography studies was followed by aortobifemoral artery bypass surgery. Although the arterial patency was restored after the operation, she did not recover from post-operative respiratory complications. Screening of PAOD is necessary for DM1 with general risk factors of occlusive arteriopathy. However, surgery should be reserved for the most severe cases.
MeSH Terms
Figure
Reference
-
1. Rakocevic Stojanovic V, Peric S, Lavrnic D, Popovic S, Ille T, Stevic Z, et al. Leptin and the metabolic syndrome in patients with myotonic dystrophy type 1. Acta Neurol Scand. 2010; 121:94–98. PMID: 19804472.
Article2. Savkur RS, Philips AV, Cooper TA. Aberrant regulation of insulin receptor alternative splicing is associated with insulin resistance in myotonic dystrophy. Nat Genet. 2001; 29:40–47. PMID: 11528389.
Article3. Udd B, Krahe R. The myotonic dystrophies: molecular, clinical, and therapeutic challenges. Lancet Neurol. 2012; 11:891–905. PMID: 22995693.
Article4. Udd B, Meola G, Krahe R, Wansink DG, Bassez G, Kress W, et al. Myotonic dystrophy type 2 (DM2) and related disorders report of the 180th ENMC workshop including guidelines on diagnostics and management 3-5 December 2010, Naarden, The Netherlands. Neuromuscul Disord. 2011; 21:443–450. PMID: 21543227.5. Daniele A, De Rosa A, De Cristofaro M, Monaco ML, Masullo M, Porcile C, et al. Decreased concentration of adiponectin together with a selective reduction of its high molecular weight oligomers is involved in metabolic complications of myotonic dystrophy type 1. Eur J Endocrinol. 2011; 165:969–975. PMID: 21964963.
Article6. Tsai JS, Guo FR, Chen SC, Lue BH, Chiu TY, Chen CY, et al. Smokers show reduced circulating adiponectin levels and adiponectin mRNA expression in peripheral blood mononuclear cells. Atherosclerosis. 2011; 218:168–173. PMID: 21605866.7. Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline). Vasc Med. 2011; 16:452–476. PMID: 22128043.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accidentally Diagnosed Myotonic Dystrophy after Cholecystectomy
- Radiofrequency Catheter Ablation of Persistent Atrial Fibrillation with Myotonic Dystrophy and Achalasia-like Esophageal Dilatation
- Myotonic Dystrophy (A case report)
- Myotonic Dystrophy Type 1 With Brain MRI Lesions Involving White Matters in Anterior Temporal Pole and Insula
- A Case of Myotonic Dystrophy with Prolonged Atrial Flutter