J Korean Med Assoc.
2006 Sep;49(9):799-805. 10.5124/jkma.2006.49.9.799.
Endobronchial Tuberculosis
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Korea. heechung@snu.ac.kr
- KMID: 2137820
- DOI: http://doi.org/10.5124/jkma.2006.49.9.799
Abstract
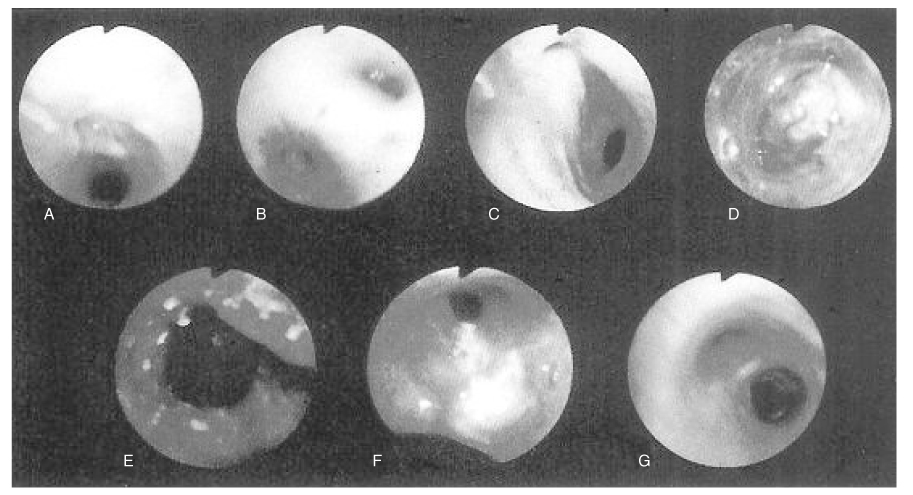
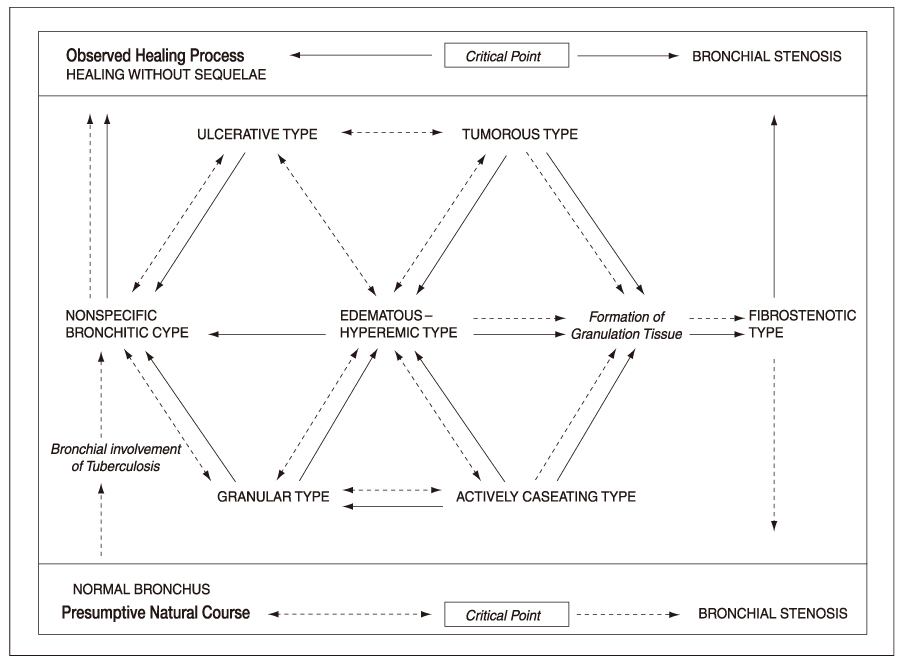
- Endobronchial tuberculosis is defined as a specific inflammation of the trachea or major bronchi caused by tubercle bacilli. Active disease can be diagnosed when certain endobronchial lesions-such as whitish gelatinous material, ulcer, tumor, stenosis, or inflammation-exist on bronchoscopy and tuberculosis is proven by bronchoscopic biopsy of these lesions. In pulmonary tuberculosis, resected lung specimens frequently show either ulceration or stenosis of the draining bronchioles or bronchi, and the same endobronchial processes may result in bronchiectasis due to destruction of the bronchial wall. These lesions are included in the disease entity of pulmonary tuberculosis rather than that of endobronchial tuberculosis because those endobronchial lesions distal to lobar bronchi do not have clinical significance. Fibrotic stenosis of bronchi may be inactive lesions resulting from prior endobronchial tuberculosis though sputum examination for acid-fast bacilli is positive, since the sequela of endobronchial tuberculosis and reactivated pulmonary tuberculosis can be present coincidentally. Therefore, it is necessary to obtain histologic proof of tuberculosis for a definite diagnosis of endobronchial tuberculosis. Endobronchial tuberculosis is a specific form or a significant complication of pulmonary tuberculosis, and it frequently causes matters of grave concern; (1) delay in diagnosis, (2) misdiagnosis as bronchial asthma, and (3) bronchial stenosis. The human immunodeficiency virus (HIV) epidemic and multidrug-resistant strains of tubercle bacilli may be associated with a higher incidence of endobronchial tuberculosis. Therefore, endobronchial tuberculosis continues to be a health problem, though the incidence of tuberculosis affecting respiratory organs including the trachea and bronchi has been greatly reduced. Endobronchial tuberculosis should be borne in mind when patients are young female adults or adolescents who present with symptoms suggestive of asthma and/or with unusual roentgenographic patterns, or in patients with HIV infection.
MeSH Terms
Figure
Cited by 1 articles
-
Endobronchial Tuberculosis Presenting as Right Middle Lobe Syndrome: Clinical Characteristics and Bronchoscopic Findings in 22 Cases
Ho Cheol Kim, Hyeon Sik Kim, Seung Jun Lee, Yi Yeong Jeong, Kyoung-Nyeo Jeon, Jong Deok Lee, Young Sil Hwang
Yonsei Med J. 2008;49(4):615-619. doi: 10.3349/ymj.2008.49.4.615.
Reference
-
1. Chung HS. Madkour MM, editor. Endobronchial tuberculosis. Tuberculosis. 2004. 1st ed. Berlin: Springer;329–348.
Article2. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000. 117:385–392.
Article3. Lerner BH. Catching patients: tuberculosis and detention in the 1990s. Chest. 1999. 115:236–241.
Article4. Calpe JL, Chiner E, Larramendi CH. Endobronchial tuberculosis in HIV-infected patients. AIDS. 1995. 9:1159–1164.
Article5. Smith LS, Schillaci RF, Sarlin RF. Endobronchial tuberculosis: serial fiberoptic bronchoscopy and natural history. Chest. 1987. 91:644–647.6. Medlar EM. The behavior of pulmonary tuberculous lesion: a pathological study. American Review of Tuberculosis. 1955. 71:132–145.7. Shulutko ML, Kazak TI, Tarasov AS. Lukomsky GI, editor. Tuberculosis. Bronchology. 1979. St Louis: Mosby;287–305.8. Chung HS, Lee JH, Han SK, Shim Y, Kim KY, Kim WS, et al. Classification of endobronchial tuberculosis by the bronchoscopic features. Tuberculosis and Respiratory Disease. 1991. 38:108–115.
Article9. Lee JH, Park SS, Lee DH, Shin DH, Yang SC, Yoo BM. Endobronchial tuberculosis: clinical and bronchoscopic features in 121 cases. Chest. 1992. 102:990–994.10. Lee JH, Chung HS. Bronchoscopic, radiologic and pulmonary function evaluation of endobronchial tuberculosis. Respirology. 2000. 5:411–418.
Article11. Ip MS, So SY, Lam WK, Mok CK. Endobronchial tuberculosis revisited. Chest. 1986. 89:727–731.
Article12. Chung HS, Lee JH. Study about the clinical features and pulmonary function test of endobronchial tuberculosis. Tuberculosis and Respiratory Disease. 1996. 43:147–158.
Article13. Kim YH, Kim HT, Lee KS, Uh ST, Cung YT, Park CS. Serial fiberoptic bronchoscopic observations of endobronchial tuberculosis before and early after antituberculosis chemotherapy. Chest. 1993. 103:673–677.
Article14. Park IW, Choi BW, Hue SH. Prospective study of corticosteroid as an adjunct in the treatment of endobronchial tuberculosis in adults. Respirology. 1997. 2:275–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of bronchomalacia due to endobronchial tuberculosis
- A case of endobronchial tuberculosis accompanied with obstructive emphysema
- A case of tumorous type of endobronchial tuberculosis simulating bronchial adenoma
- Clinical Course of Endobrochial Tuberculosis Diagnosed by Flexible Bronchoscopy in Children
- The Clinical Significances of Bronchial Anthracofibrosis in the Patients with Endobronchial Tuberculosis