J Korean Med Assoc.
2008 Nov;51(11):992-1006. 10.5124/jkma.2008.51.11.992.
Vestibular Neuritis and Bilateral Vestibulopathy
- Affiliations
-
- 1Department of Neurology, Pusan National University Medical School, Korea. choikwangdong@hanmail.net
- 2Department of Otolaryngology, Pusan National University Medical School, Korea. gohek@pusan.ac.kr
- KMID: 2137742
- DOI: http://doi.org/10.5124/jkma.2008.51.11.992
Abstract
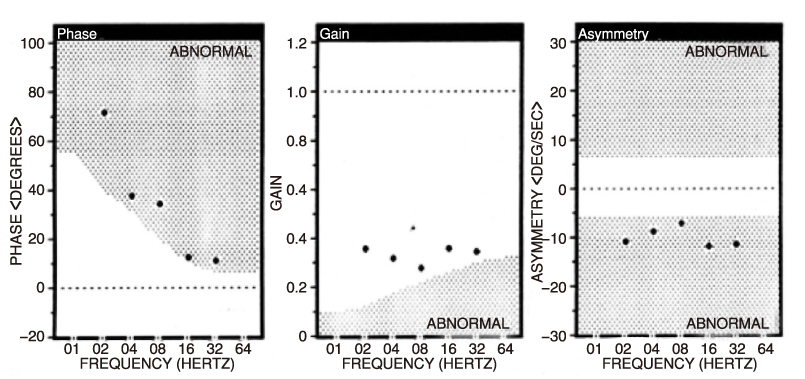
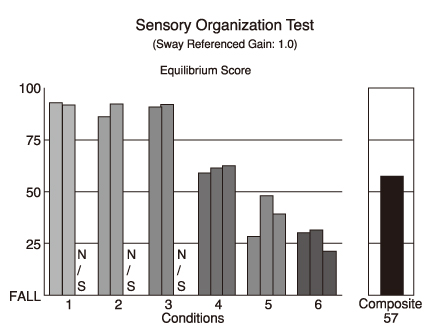
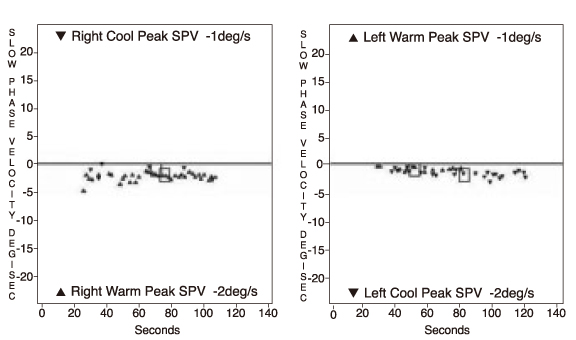
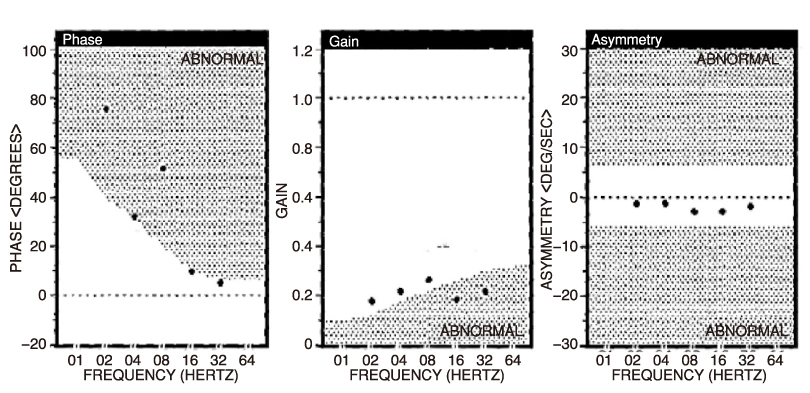
- Vestibular neuritis is the second most common cause of peripheral vestibular vertigo. The key signs and symptoms are the acute onset of sustained rotatory vertigo without hearing loss, postural imbalance with Romberg's sign, and peripheral type nystagmus. Head thrust and caloric tests show ipsilateral hyporesponsiveness, but hearing test shows normal. Either an inflammation of the vestibular nerve or labyrinthine ischemia was proposed as a cause of vestibular neuritis. Recovery after vestibular neuritis is usually incomplete. Despite the assumed viral cause, the effects of corticosteroids, antiviral agents, or the two in combination are uncertain. Bilateral vestibulopathy is a rare disorder of the peripheral labyrinth or the eighth nerve. The most frequent etiologies include ototoxicity, autoimmune disorders, meningitis, neuropathies, sequential vestibular neuritis, cerebellar degeneration, tumors, and miscellaneous otological diseases. The two key symptoms are unsteadiness of gait and oscillopsia associated with head movements or when walking. The diagnosis is made with the simple bedside tests for defective vestibulo-ocular reflex (head thrust and dynamic visual acuity tests). Bilateral vestibulopathy is confirmed by the absence of nystagmus reaction to both caloric and rotatory chair tests. The spontaneous recovery is relatively rare and incomplete. Vestibular rehabilitation is supportive of the improvement, but the efficacy of physical therapy is limited.
MeSH Terms
Figure
Reference
-
1. Leigh RJ, Zee DS, editors. The neurology of eye movements. 2006. 4th ed. New York: Oxford University;20–81.2. Goldberg JM, Fernandez C. Physiology of peripheral neurons innervating semicircular canals of the squirrel monkey. I. Resting discharge and response to constant angular acceleration. J Neurophysiol. 1971. 34:635–660.
Article3. Miles FA, Braitman DJ. Long-term adaptive changes in primate vestibuloocular reflex. II. Electrophysiological observations on semicircular canal primary afferents. J Neurophysiol. 1980. 43:1426–1436.
Article4. Baloh RW. Clinical practice. Vestibular neuritis. N Engl J Med. 2003. 348:1027–1032.5. Rinne T, Bronstein AM, Rudge P, Gresty MA, Luxon LM. Bilateral loss of vestibular function. Acta Otolaryngol. 1995. 520:247–250.
Article6. Kroenke K, Hoffman RM, Einstadter D. How common are various causes of dizziness?: A critical review. S Med J. 2000. 93:160–167.
Article7. Nedzelski JM, Barber HO, McIlmoyl L. Diagnosis in a dizziness unit. J Otolaryngol. 1986. 15:101–104.8. Baloh RW, Halmagyi GM, editors. Disorders of the vestibular system. 1996. New York: Oxford University;318–327.9. Choi KD, Oh SY, Kim HJ, Koo JW, Cho BM, Kim JS. Recovery of vestibular imbalances after vestibular neuritis. Laryngoscope. 2007. 117:1307–1312.
Article10. Safran AB, Vibert D, Issoua D, Hausler R. Skew deviation after vestibular neuritis. Am J Ophthalmol. 1994. 118:238–245.
Article11. Furman JM, Cass SP, editors. Vestibular disorders: a case-study approach. 2003. 3rd ed. New York: FA Davis;21–29.12. Halmagyi GM, Curthoys IS. A clinical sign of canal paresis. Arch Neurol. 1988. 45:737–739.
Article13. Schubert MC, Tusa RJ, Grine LE, Herdman SJ. Optimizing the sensitivity of the head thrust test for identifying vestibular hypofunction. Phys Ther. 2004. 84:151–158.
Article14. Cremer PD, Halmagyi GM, Aw ST, Curthoys IS, McGarvie LA, Todd MJ, Black RA, Hannigan IP. Semicircular canal plane head impulses detect absent function of individual semicircular canals. Brain. 1998. 121:699–716.
Article15. Colebatch JG, Halmagyi GM, Skuse NF. Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry. 1994. 57:190–197.
Article16. Murofushi T, Halmagyi GM, Yavor RA, Colebatch JG. Absent vestibular evoked myogenic potentials in vestibular neurolabyrinthitis. An indicator of inferior vestibular nerve involvement? Arch Otolaryngol Head Neck Surg. 1996. 122:845–848.
Article17. Hilding DA, Kanda T, House WF. Vestibular neuronitis and small acoustic neuroma: electron microscopic observations. Otol Clin N Am. 1968. 1:305–318.
Article18. Schuknecht HF, Kitamura K, Louis H Second. Clerf lecture, Vestibular neuritis. Ann Otol Rhinol Laryngol Suppl. 1981. 90:1–19.19. Hirata T, Sekitani T, Okinaka Y, Matsuda Y. Serovirological study of vestibular neuronitis. Acta Otolaryngol Suppl. 1989. 468:371–373.
Article20. Kim JS, Lopez I, DiPatre PL, Liu F, Ishiyama A, Baloh RW. Internal auditory artery infarction: clinicopathologic correlation. Neurology. 1999. 52:40–44.
Article21. Fetter M, Dichgans J. Vestibular neuritis spares the inferior division of the vestibular nerve. Brain. 1996. 119:755–763.
Article22. Hotson JR, Baloh RW. Acute vestibular syndrome. N Engl J Med. 1998. 339:680–685.
Article23. Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ. Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis. Neurology. 2008. 70:2378–2385.
Article24. Selesnick SH, Jackler RK, Pitts LW. The changing clinical presentation of acoustic tumors in the MRI era. Laryngoscope. 1993. 103:431–436.
Article25. Ishikawa K, Edo M, Togawa K. Clinical observation of 32 cases of vestibular neuronitis. Acta Otolaryngol Suppl. 1993. 503:13–15.
Article26. Okinaka Y, Sekitani T, Okazaki H, Miura M, Tahara T. Progress of caloric response of vestibular neuronitis. Acta Otolaryngol Suppl. 1993. 503:18–22.
Article27. Bergenius J, Perols O. Vestibular neuritis: a follow-up study. Acta Otolaryngol. 1999. 119:895–899.
Article28. Meran A, Pfaltz CR. The acute vestibular paralysis. Arch Otorhinolaryngol. 1975. 209:229–244.29. Cameron SA, Dutia MB. Lesion-induced plasticity in rat vestibular nucleus neurones dependent on glucocorticoid receptor activation. J Physiol. 1999. 518:151–158.
Article30. Kitahara T, Kondoh K, Morihana T, Okumura S, Horii A, Takeda N, Kubo T. Steroid effects on vestibular compensation in human. Neurol Res. 2003. 25:287–291.
Article31. Strupp M, Zingler VC, Arbusow V, Niklas D, Maag KP, Dieterich M, Bense S, Theil D, Jahn K, Brandt T. Methylprednisolone, valacyclovir, or the combination for vestibular neuritis. N Engl J Med. 2004. 351:354–361.
Article32. Cooksey FS. Rehabilitation in vestibular injury. Proc R Soc Med. 1946. 39:273–278.33. Viber D, liard P, Hausler R. Bilateral idiopathic loss of peripheral vestibular function with normal hearing. Acta Otolaryngol. 1995. 115:611–615.
Article34. Dandy WE. The surgical treatment of Meniere's disease. Surg Gynecol Obstet. 1941. 72:421–425.35. Bhansali SA, Stockwell CW, Bojrab DI. Oscillopsia in patients with loss of vestibular function. Otolaryngol Head Neck Surg. 1993. 109:120–126.
Article36. Chamber BR, Mai M, Barber HO. Bialteral vestibular loss, oscillopsia, and the cervico-ocular reflex. Otolaryngol Head Neck Surg. 1985. 93:403–407.37. Mayer E, Bernstein J, Fostiropolous G. Salicylate ototoxicity. A clinical study. N Engl J Med. 1965. 273:587.38. Rinne T, Bronstein AM, Rudge P, Gresty MA, Luxon LM. Bilateral loss of vestibular function: clinical findings in 53 patients. J Neurol. 1998. 245:314–321.
Article39. McGath JH, Barber HO, Stoyanoff S. Bilateral vestibular loss and oscillopsia. J Otolaryngol. 1989. 18:218–221.40. Furman JM, Kamerer DB. Rotational responses in patients with bilateral caloric reduction. Acta Otolaryngol. 1989. 108:355–361.
Article41. Rinne T, Bronstein AM, Rudge P, Gresty MA, Luxon LM. Bilateral loss of vestibular function. Acta Otolaryngol. 1995. 520:247–250.
Article42. Gillespie MB, Minor LB. Prognosis in bilateral vestibular hypofunction. Laryngoscope. 1999. 109:35–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Vestibular Hypofunction Induced by Unilateral Herpes Zoster Oticus
- A Case of Benign Paroxysmal Positional Vertigo and Sudden Hearing Loss during Recovery Phase of Vestibular Neuritis
- Clinical Application of Video Head Impulse Test in Acute Vestibular Syndrome
- A Case of Isolated Nodular Infarction Mimicking Vestibular Neuritis on the Contralateral Side
- A Case of Facial Palsy Developed after Vestibular Neuritis Involving Superior Vestibular Nerve