J Korean Med Assoc.
2009 Jan;52(1):14-21. 10.5124/jkma.2009.52.1.14.
Radiologic Diagnosis of Interstitial Lung Diseases
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. kyungs.lee@samsung.com
- KMID: 2137729
- DOI: http://doi.org/10.5124/jkma.2009.52.1.14
Abstract
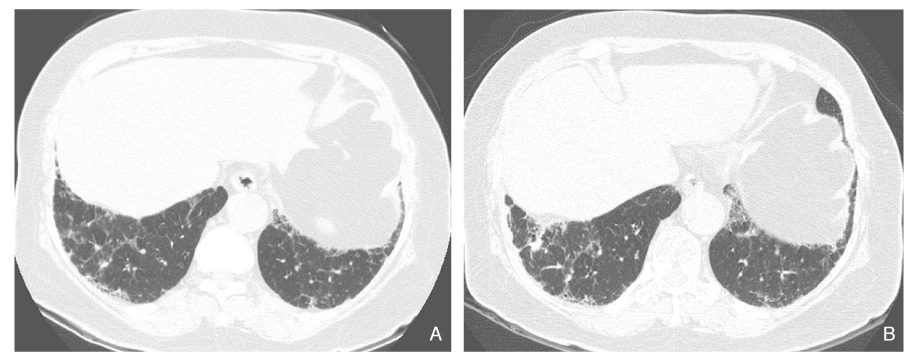
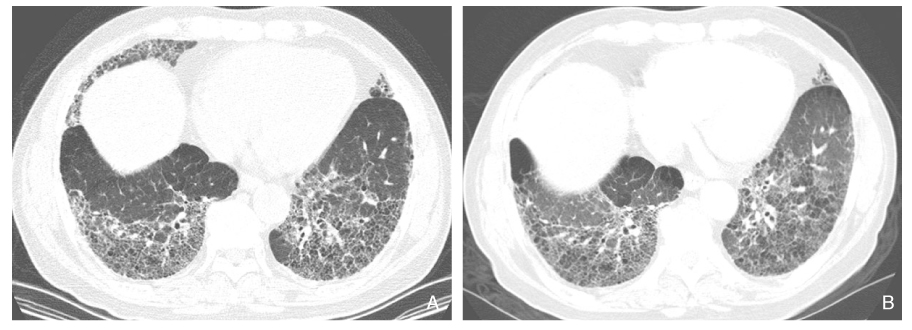
- Diffuse interstitial lung diseases (DILD) are a group of chronic disorders showing varying degrees of active inflammation and established fibrosis mainly involving the interstitium of the lungs. DILD can be classified into two groups in an etiologic aspect; idiopathic and DILD with known-cause, such as connective tissue diseases associated with DILD. Although there had been complexity and variability in the classification of idiopathic interstitial pneumonia (IIP), an international standard was established for the classification of IIPs including seven clinicalradiologic-pathologic entities; idiopathic pulmonary fibrosis (IPF), nonspecific interstitial pneumonia (NSIP), cryptogenic organizing pneumonia (COP), acute interstitial pneumonia (AIP), respiratory bronchiolitis-associated interstitial lung disease (RB-ILD), desquamative interstitial pneumonia (DIP), and lymphoid interstitial pneumonia (LIP). The prognosis of fibrotic NSIP and IPF is much poorer compared to those of other spectrum of IIPs, such as COP, RB-ILD, DIP, and LIP. Therefore, fibrotic NSIP and IPF can be considered separately as a group of fibrotic IIPs. Trying to predict the prognosis of IIPs, there has been an effort to differentiate inflammationpredominant lesions from fibrosis-predominant lesions in patients with fibrotic IIPs. Radiologic features of low fibrotic scores at high-resolution CT and early enhancement patterns at dynamic enhancement of MRI can be useful prognostic determinants for the prediction of disease improvement in patients with fibrotic IIPs.
Keyword
MeSH Terms
Figure
Reference
-
1. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002. 165:277–304.2. Demedts M, Costabel U. ATS/ERS international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Eur Respir J. 2002. 19:794–796.
Article3. Monaghan H, Wells AU, Colby TV, du Bois RM, Hansell DM, Nicholson AG. Prognostic implications of histologic patterns in multiple surgical lung biopsies from patients with idiopathic interstitial pneumonias. Chest. 2004. 125:522–526.
Article4. Flaherty KR, Toews GB, Travis WD, Colby TV, Kazerooni EA, Gross BH, Jain A, Strawderman RL 3rd, Paine R, Flint A, Lynch JP 3rd, Martinez FJ. Clinical significance of histological classification of idiopathic interstitial pneumonia. Eur Respir J. 2002. 19:275–283.
Article5. Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, Offord KP. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998. 157:199–203.
Article6. Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, Jain A, Strawderman RL, Flint A, Lynch JP, Martinez FJ. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001. 164:1722–1727.
Article7. Qureshi RA, Ahmed TA, Grayson AD, Soorae AS, Drakeley MJ, Page RD. Does lung biopsy help patients with interstitial lung disease? Eur J Cardiothorac Surg. 2002. 21:621–626. discussion 626.
Article8. Lettieri CJ, Veerappan GR, Parker JM, Franks TJ, Hayden D, Travis WD, Shorr AF. Discordance between general and pulmonary pathologists in the diagnosis of interstitial lung disease. Respir Med. 2005. 99:1425–1430.
Article9. Hunninghake GW, Lynch DA, Galvin JR, Gross BH, Muller N, Schwartz DA, King TE Jr, Lynch JP 3rd, Hegele R, Waldron J, Colby TV, Hogg JC. Radiologic findings are strongly associated with a pathologic diagnosis of usual interstitial pneumonia. Chest. 2003. 124:1215–1223.
Article10. MacDonald SL, Rubens MB, Hansell DM, Copley SJ, Desai SR, du Bois RM, Nicholson AG, Colby TV, Wells AU. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparative appearances at and diagnostic accuracy of thin-section CT. Radiology. 2001. 221:600–605.
Article11. Lee JS, Im JG, Ahn JM, Kim YM, Han MC. Fibrosing alveolitis: prognostic implication of ground-glass attenuation at high-resolution CT. Radiology. 1992. 184:451–454.
Article12. Shin KM, Lee KS, Chung MP, Han J, Bae YA, Kim TS, Chung MJ. Prognostic determinants among clinical, thin-section CT, and histopathologic findings for fibrotic idiopathic interstitial pneumonias: tertiary hospital study. Radiology. 2008. 249:328–337.
Article13. Riha RL, Duhig EE, Clarke BE, Steele RH, Slaughter RE, Zimmerman PV. Survival of patients with biopsy-proven usual interstitial pneumonia and nonspecific interstitial pneumonia. Eur Respir J. 2002. 19:1114–1118.
Article14. Flaherty KR, Thwaite EL, Kazerooni EA, Gross BH, Toews GB, Colby TV, Travis WD, Mumford JA, Murray S, Flint A, Lynch JP 3rd, Martinez FJ. Radiological versus histological diagnosis in UIP and NSIP: survival implications. Thorax. 2003. 58:143–148.
Article15. Hartman TE, Swensen SJ, Hansell DM, Colby TV, Myers JL, Tazelaar HD, Nicholson AG, Wells AU, Ryu JH, Midthun DE, du Bois RM, Muller NL. Nonspecific interstitial pneumonia: variable appearance at high-resolution chest CT. Radiology. 2000. 217:701–705.
Article16. Gaeta M, Blandino A, Scribano E, Minutoli F, Barone M, Ando F, Pandolfo I. Chronic infiltrative lung diseases: value of gadolinium-enhanced MRI in the evaluation of disease activity-early report. Chest. 2000. 117:1173–1178.17. Yi CA, Lee KS, Han J, Chung MP, Chung MJ, Shin KM. 3-T MRI for differentiating inflammation-and fibrosis-predominant lesions of usual and nonspecific interstitial pneumonia: comparison study with pathologic correlation. Ajr. 2008. 190:878–885.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Radiologic Approach to Diffuse Interstitial Lung Disease
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Update in Diagnosis of Idiopathic Pulmonary Fibrosis and Interstitial Lung Abnormality
- The Comparision of the Clinical, Laboratory and Radiologic Factors in Rheumatoid Arthritis Patients with or Without Interstitial Lung Disease
- Radiologic Approach to the Idiopathic Interstitial Pneumonias