Brain Tumor Res Treat.
2014 Oct;2(2):132-137. 10.14791/btrt.2014.2.2.132.
Brain Metastases of Papillary Thyroid Carcinoma with Horner's Syndrome
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, The Catholic University of Korea, Yeouido St. Mary's Hospital, Seoul, Korea. jwi@catholic.ac.kr
- KMID: 2134286
- DOI: http://doi.org/10.14791/btrt.2014.2.2.132
Abstract
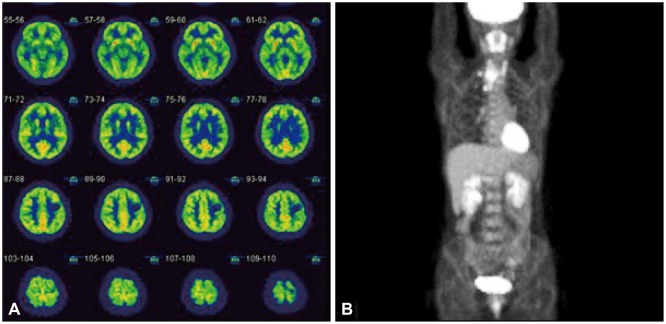
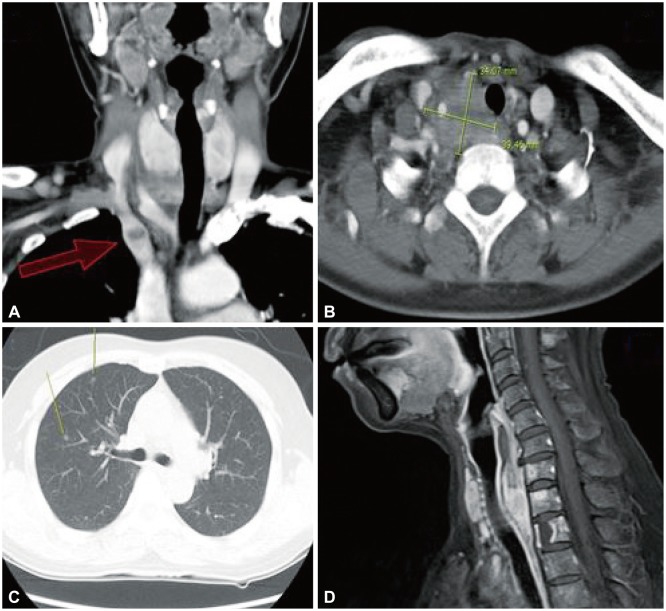
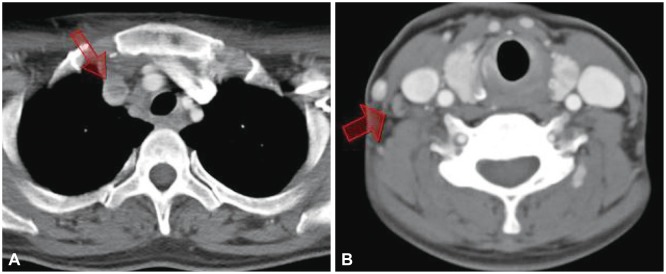
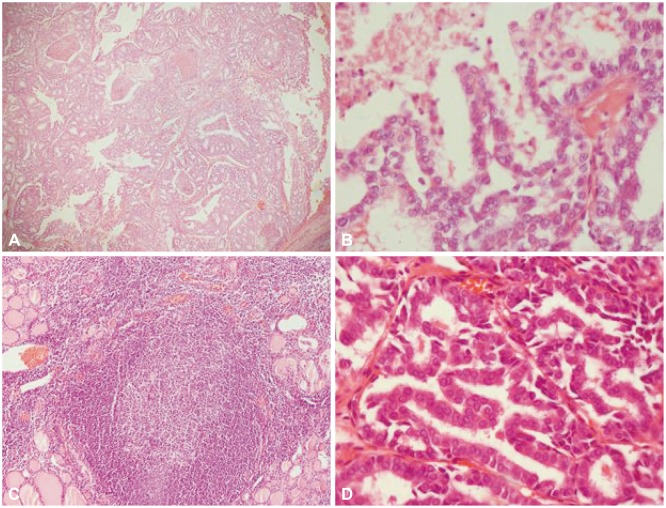
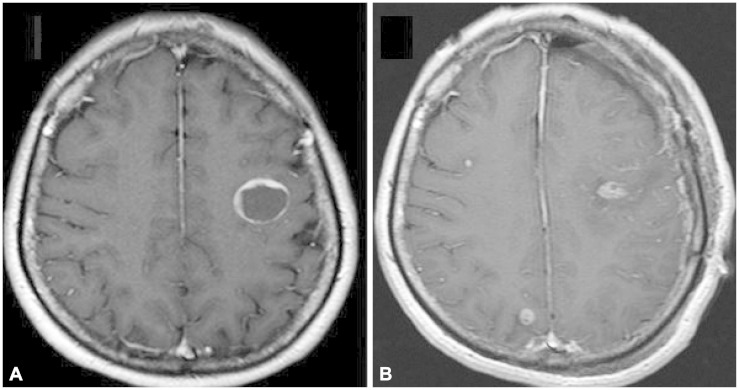
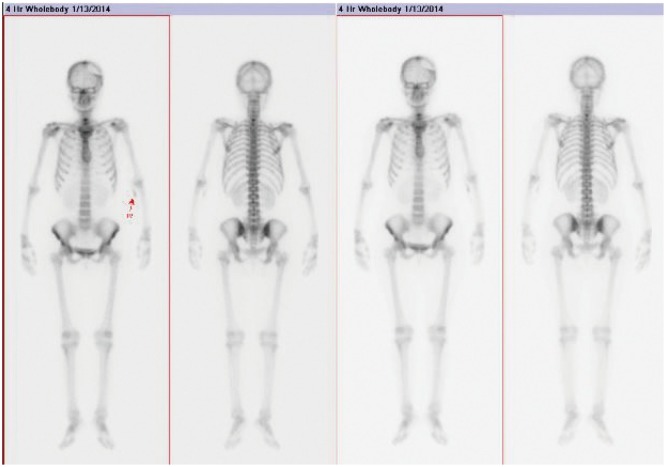
- Papillary thyroid carcinoma (PTC) is the most common type of thyroid malignancy and has relatively favorable prognosis. Blood-borne metastases of PTC are very rare among the thyroid malignancies. Moreover a case of blood-borne central nervous system metastasized PTC with only unilateral Horner's syndrome, and without any abnormalities in laboratory or physical examinations has not been described before. A 53-year-old female patient had been managed in ophthalmologic clinic due to vague symptoms of right monocular blurred vision with eye dryness for 3 months, but showed no signs of improvement. So it was performed a magnetic resonance imaging and magnetic resonance angiography to evaluate the possibilities of cerebral lesion. And a left frontal mass was incidentally found, and the tumor turned out to be a PTC that had metastasized to brain, regional lymph node, cervical, thoracic spine, and lung. We describe a PTC with extraordinary initial symptoms that metastasized to an unusual site. We recommend that if a papillary thyroid tumor with unusual symptoms or at an advanced stage is found, further investigation should be performed for distant metastasis.
MeSH Terms
Figure
Reference
-
1. Miranda ER, Padrão EL, Silva BC, De Marco L, Sarquis MS. Papillary thyroid carcinoma with brain metastases: an unusual 10-year-survival case. Thyroid. 2010; 20:657–661. PMID: 20470207.
Article2. McCaffrey TV, Bergstralh EJ, Hay ID. Locally invasive papillary thyroid carcinoma: 1940-1990. Head Neck. 1994; 16:165–172. PMID: 8021137.
Article3. Gauden AJ, Gauden SJ. Multiple cerebral metastases as a primary presentation in papillary thyroid carcinoma. J Clin Neurosci. 2010; 17:379–380. PMID: 20074955.
Article4. Harding JL, Sywak MS, Sidhu S, Delbridge LW. Horner's syndrome in association with thyroid and parathyroid disease. ANZ J Surg. 2004; 74:442–445. PMID: 15191478.
Article5. Broome JT, Gauger PG, Miller BS, Doherty GM. Anaplastic thyroid cancer manifesting as new-onset Horner syndrome. Endocr Pract. 2009; 15:563–566. PMID: 19491063.
Article6. Tahmasebi FC, Farmer P, Powell SZ, et al. Brain metastases from papillary thyroid carcinomas. Virchows Arch. 2013; 462:473–480. PMID: 23532501.
Article7. Mazzaferri EL, Young RL, Oertel JE, Kemmerer WT, Page CP. Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore). 1977; 56:171–196. PMID: 859443.8. Yamagami Y, Tori M, Sakaki M, Ohtake S, Nakahara M, Nakao K. Thyroid carcinoma with extensive tumor thrombus in the atrium. Gen Thorac Cardiovasc Surg. 2008; 56:555–558. PMID: 19002756.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Papillary Thyroid Cancer Arising in Lateral Aberrant Thyroid Presenting with Multiple Metastases
- Painful Horner syndrome after thyroidectomy: A case report
- Brain Metastasis from Papillary Carcinoma of the Thyroid
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Occult Papillary Thyroid Carcinoma Presenting as a Metastatic Pleural Effusion