J Vet Sci.
2015 Dec;16(4):517-523. 10.4142/jvs.2015.16.4.517.
Chitosan hemostatic dressing for control of hemorrhage from femoral arterial puncture site in dogs
- Affiliations
-
- 1Department of Clinical Sciences of Companion Animals, Faculty of Veterinary Medicine, Utrecht University, 3584 CM Utrecht, The Netherlands. v.szatmari@uu.nl
- KMID: 2133635
- DOI: http://doi.org/10.4142/jvs.2015.16.4.517
Abstract
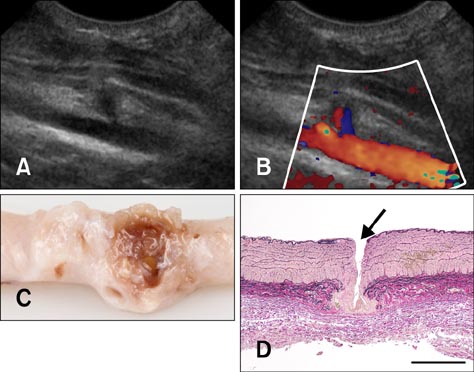
- Removal of an introducer-sheath from a femoral artery after completing transarterial embolization of a patent ductus arteriosus can cause life-threatening hemorrhage in dogs. In the present study, the effectiveness of chitosan acetate dressing in 10 experimental dogs was tested. Under general anesthesia, an introducer-sheath was placed into the femoral artery with percutaneous puncture using Seldinger's technique. The outer diameter of the introducer-sheaths varied from 3.0 to 4.0 mm with an introducer/artery ratio of 80 to 123%. The artery's diameter was measured using ultrasonography. Following removal of the introducer-sheath, a chitosan acetate dressing was applied to the wound and held in place with manual compression for 10 min. Successful hemostasis was reached on 12 arteries. However, on two arteries, hemorrhage was uncontrollable and led to a hypovolemic shock during 10 min of manual compression. Possible causes of the negative outcome in two dogs were their old age and an introducer-sheath with a too large diameter. The chitosan acetate dressing was easy to use and the artery remained patent. Dogs could walk directly after recovery from anesthesia and their femoral arteries were saved. In conclusion, the outer diameter of the introducer-sheath should not exceed 3 mm or the inner diameter of the artery.
MeSH Terms
Figure
Reference
-
1. Aksoy M, Becquemin JP, Desgranges P, Allaire E, Kobeiter H. The safety and efficacy of angioseal in therapeutic endovascular interventions. Eur J Vasc Endovasc Surg. 2006; 32:90–93.
Article2. Arbel J, Rozenbaum E, Reges O, Neuman Y, Levi A, Erel J, Haskia AR, Caneti M, Sherf M, Mosseri M. Usage of chitosan for femoral (USF) haemostasis after percutaneous procedures: a comparative open label study. EuroIntervention. 2011; 6:1104–1109.
Article3. Beal MW, Hughes D. Vascular access: theory and techniques in the small animal emergency patient. Clin Tech Small Anim Pract. 2000; 15:101–109.
Article4. Burkatovskaya M, Castano AP, Demidova-Rice TN, Tegos GP, Hamblin MR. Effect of chitosan acetate bandage on wound healing in infected and noninfected wounds in mice. Wound Repair Regen. 2008; 16:425–431.
Article5. Caivano D, Birettoni F, Fruganti A, Rishniw M, Knafelz P, Moïse NS, Porciello F. Transthoracic echocardiographically-guided interventional cardiac procedures in the dog. J Vet Cardiol. 2012; 14:431–444.
Article6. Devlin JJ, Kircher S, Kozen BG, Littlejohn LF, Johnson AS. Comparison of ChitoFlex, CELOX, and QuikClot in control of hemorrhage. J Emerg Med. 2011; 41:237–245.
Article7. Gargiulo NJ 3rd, Veith FJ, Ohki T, Scher LA, Berdejo GL, Lipsitz EC, Menegus M, Greenberg M. Histologic and duplex comparison of the perclose and angio-seal percutaneous closure devices. Vascular. 2007; 15:24–29.
Article8. Klokkevold PR, Fukayama H, Sung EC, Bertolami CN. The effect of chitosan (poly-N-acetyl glucosamine) on lingual hemostasis in heparinized rabbits. J Oral Maxillofac Surg. 1999; 57:49–52.
Article9. MacIntyre AD, Quick JA, Barnes SL. Hemostatic dressings reduce tourniquet time while maintaining hemorrhage control. Am Surg. 2011; 77:162–165.
Article10. Nguyenba TP, Tobias AH. The Amplatz canine duct occluder: a novel device for patent ductus arteriosus occlusion. J Vet Cardiol. 2007; 9:109–117.
Article11. Sanghi P, Virmani R, Do D, Erikson J, Elliott J, Cilingiroglu M, Matthews H, Kazi M, Ricker R, Bailey SR. A comparative evaluation of arterial blood flow and the healing response after femoral artery closure using angioseal STS Plus and StarClose in a porcine model. J Interv Cardiol. 2008; 21:329–336.
Article12. Schneider M, Schneider I, Hildebrandt N, Wehner M. Percutaneous angiography of Patent Ductus Arteriosus in dogs: techniques, results and implications for intravascular occlusion. J Vet Cardiol. 2003; 5:21–27.
Article13. Schwartz RB, Reynolds BZ, Shiver SA, Lerner EB, Greenfield EM, Solis RA, Kimpel NA, Coule PL, McManus JG. Comparison of two packable hemostatic Gauze dressings in a porcine hemorrhage model. Prehosp Emerg Care. 2011; 15:477–482.
Article14. Thatte HS, Zagarins SE, Amiji M, Khuri SF. Poly-N-acetyl glucosamine-mediated red blood cell interactions. J Trauma. 2004; 57:Suppl. S7–S12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Recombinant Human Epidermal Growth Factor Impregnated Chitosan Film on Hemostasis and Healing of Blood Vessels
- Evaluation of the Optimal Site for Retrograde Common Femoral Arterial Puncture
- Experimental Assessment of Hemostatic Agents: Comparison with New Developed Chitosan-Based Material
- Wound Healing Effect of the Chitosan Sponge
- Chitosan Pad, Cellulose Membrane, or Gelatin Sponge for Peridural Bleeding: An Efficacy Study on a Lumbar Laminectomized Rat Model