Ann Clin Microbiol.
2015 Dec;18(4):111-118. 10.5145/ACM.2015.18.4.111.
Comparison of Antibiotic Resistance Rate of Medically Important Microorganisms between Japan and Korea
- Affiliations
-
- 1Department of Bacteriology II, National Institute of Infectious Diseases, Tokyo, Japan.
- 2Department of Laboratory Medicine, Catholic Kwangdong University, Incheon, Korea.
- 3Department of Laboratory Medicine, Gyeongsang National University School of Medicine, Gyeongsang Health Science Institute, Jinju, Korea. sjkim8239@hanmail.net
- KMID: 2133607
- DOI: http://doi.org/10.5145/ACM.2015.18.4.111
Abstract
- BACKGROUND
A surveillance system for antibiotic resistance is well organized in both Japan and Korea; however, a comparative analysis by microorganism has not previously been conducted.
METHODS
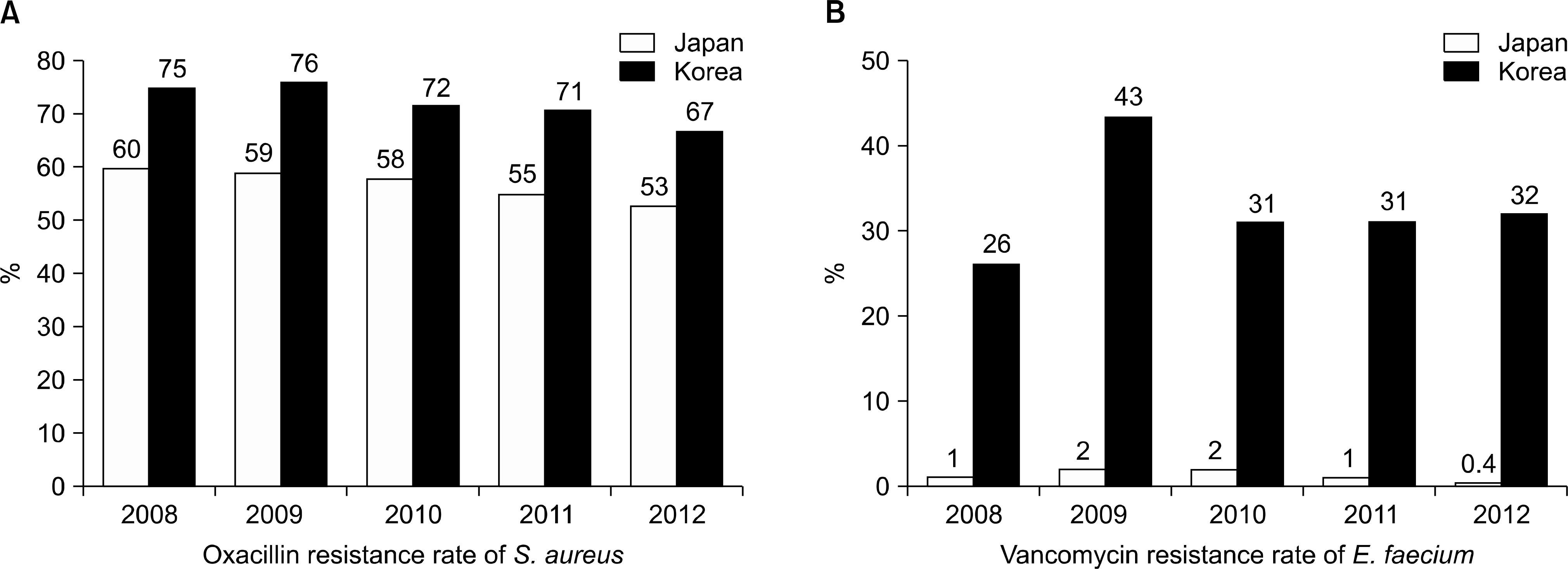
We compared the latest antibiotic resistance rates of medically important pathogens, such as Staphylococcus aureus, enterococci, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii, between Japan and Korea. Data were collected by JANIS (Japan Nosocomial Infections Surveillance) and KARMS (Korean Antimicrobial Resistance Monitoring System) from 2007-2012.
RESULTS
In 2012, the proportions of oxacillin-resistant S. aureus, vancomycin-resistant Enterococcus faecium (VRE), cefotaxime-resistant E. coli, ceftazidime-resistant K. pneumoniae, imipenem-resistant P. aeruginosa, and imipenem-resistant A. baumannii were 53%, 0.4%, 16.6%, 2.9%, 18.5%, and 2% in Japan and 67%, 32%, 29%, 40%, 28%, and 70% in Korea, respectively.
CONCLUSION
There were large differences in the frequencies of VRE, ceftazidime-resistant K. pneumoniae, and imipenem-resistant A. baumannii between Japan and Korea. A collaborative study to probe the differences in the antibiotic resistance rates between the two countries should be performed.
Keyword
MeSH Terms
Figure
Reference
-
1.Goossens H. European strategies to control antibiotic resistance and use. Ann Clin Micrbiol. 2014. 17:1–8.
Article2.Open reports of Clinical Laboratory Division of Japan Nosocomial Infections Surveillance (JANIS). http://www.nih-janis.jp/report/kensa.html. [Online] (reports in Japanese).3.Korean Antimicrobial Resistance Monitoring System (KARMS). KARMS annual report 2012. Korea National Institute of Health.4.Kwon JC., Kim SH., Park SH., Choi SM., Lee DG., Choi JH, et al. Molecular epidemiologic analysis of methicillin-resistant Staphylococcus aureus isolates from bacteremia and nasal colonization at 10 intensive care units: multicenter prospective study in Korea. J Korean Med Sci. 2011. 26:604–11.5.Song JH. Antimicrobial resistance in Gram-positive cocci: past 50 years, present and future. Infect Chemother. 2011. 43:443–9.
Article6.Park YJ., Jeong JS., Park ES., Shin ES., Kim SH., Lee YS. Survey on the infection control of multidrug-resistant microorganisms in general hospitals in Korea. Korean J Nosocomial Infect Control. 2007. 12:112–21.7.Lee K., Yong D., Jeong SH., Chong Y. Multidrug-resistant Acinetobacter spp.: increasingly problematic nosocomial pathogens. Yonsei Med J. 2011. 52:879–91.8.Yoon YK., Sim HS., Kim JY., Park DW., Sohn JW., Roh KH, et al. Epidemiology and control of an outbreak of vancomycin-resistant enterococci in the intensive care units. Yonsei Med J. 2009. 50:637–43.
Article9.Lee H., Yong D., Kim MS., Yum JH., Lee WG., Huh JY, et al. Antimicrobial susceptibities and PFGE patterns of vancomycin- resistant enterococcus isolated from clinical specimens and chi-ckens. Korean J Lab Med. 2005. 25:39–45.10.Lee K., Lee MA., Lee CH., Lee J., Roh KH., Kim S, et al. KONSAR Group. Increase of ceftazidime- and fluoroquinolone-resistant Klebsiella pneumoniae and imipenem-resistant Acinetobacter spp. in Korea: analysis of KONSAR study data from 2005 and 2007. Yonsei Med J. 2010. 51:901–11.11.Yong D., Shin HB., Kim YK., Cho J., Lee WG., Ha GY, et al. KONSAR group. Increase in the prevalence of carbapenem-re-sistant Acinetobacter isolates and ampicillin-resistant non-typhoi-dal Salmonella species in Korea: A KONSAR study conducted in 2011. Infect Chemother. 2014. 46:84–93.12.Kim NH., Hwang JH., Song KH., Choe PG., Park WB., Kim ES, et al. Changes in antimicrobial susceptibility of blood isolates in a university hospital in South Korea, 1998-2010. Infect Chemother. 2012. 44:275–81.
Article13.Kang CI., Song JH. Antimicrobial resistance in Asia: current epidemiology and clinical implications. Infect Chemother. 2013. 45:22–31.
Article14.Yoon YK., Kim MJ., Sohn JW., Park DW., Kim JY., Chun BC. Surveillance of antimicrobial use and antimicrobial resistance. Infect Chemother. 2008. 40:93–101.
Article15.Cho OH., Bak MH., Baek EH., Park KH., Kim S., Bae IG. Successful control of carbapenem-resistant Acinetobacter baumannii in a Korean university hospital: a 6-year perspective. Am J Infect Control. 2014. 42:976–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myths and Misconceptions around Antibiotic Resistance: Time to Get Rid of Them
- Antibiotic Stewardship: A Key Strategy to Combat Antibiotic Resistance
- Bacteriologic Study on Conjunctiva of Eyeball Donor and Antibiotic Sensitivity Test
- Changes in the Profiles of Causative Agents and Antibiotic Resistance Rate for Spontaneous Bacterial Peritonitis: an Analysis of Cultured Microorganisms in Recent 12 Years
- Changing pattern of microorganisms and antibiotic resistance rate of spontaneous bacterial peritonitis: A 12-year experience