Korean J Ophthalmol.
2014 Jun;28(3):213-219. 10.3341/kjo.2014.28.3.213.
Patient's Self-recognition of Reduced Visual Acuity Due to Recurrence of Macular Edema and Prompt Visitation to the Hospital in Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. kimoph@gmail.com
- 2Graduate School of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2133319
- DOI: http://doi.org/10.3341/kjo.2014.28.3.213
Abstract
- PURPOSE
To evaluate patients' self-recognition of reduced visual acuity due to recurring macular edema in retinal vein occlusion.
METHODS
A retrospective review of medical records of patients who were diagnosed with recurring macular edema secondary to retinal vein occlusion was performed. The proportion of patients who recognized reduced visual acuity due to the recurrence of macular edema and who visited the hospital before the scheduled follow-up date was determined. Parameters including age, sex, diagnosis, visual acuity before recurrence of macular edema, and extent of visual acuity reduction due to recurrence of macular edema were compared in patients who recognized a reduction in visual acuity and those who did not. The proportion of patients who visited the hospital promptly was also determined.
RESULTS
Forty eyes of 40 patients were included in the analysis. Sixteen and 24 patients were diagnosed with central retinal vein occlusion and branch retinal vein occlusion, respectively. Twenty-one patients (52.5%) recognized reduced visual acuity due to recurring macular edema. These patients were younger (59.2 +/- 7.6 vs. 64.8 +/- 9.4 years, p = 0.046), had better visual acuity before recurrence of macular edema (0.52 +/- 0.48 vs. 1.02 +/- 0.46, p = 0.002), and exhibited a greater reduction in visual acuity after recurrence of macular edema (0.34 +/- 0.24 vs. 0.14 +/- 0.13, p = 0.003). Only four patients visited the hospital before the scheduled follow-up date, and all of these patients lived relatively close to the hospital.
CONCLUSIONS
For prompt treatment of recurring macular edema, more intensive education about the self-estimation of visual acuity is necessary, particularly for elderly patients who have relatively poor visual acuity. In addition, a simple and easy way to identify the recurrence of macular edema at the local clinic should be established for patients who live relatively far from the hospital.
MeSH Terms
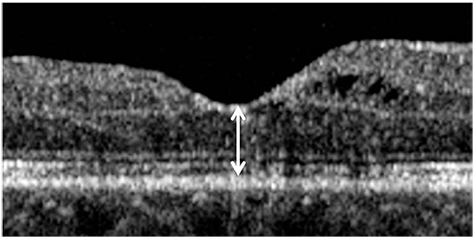
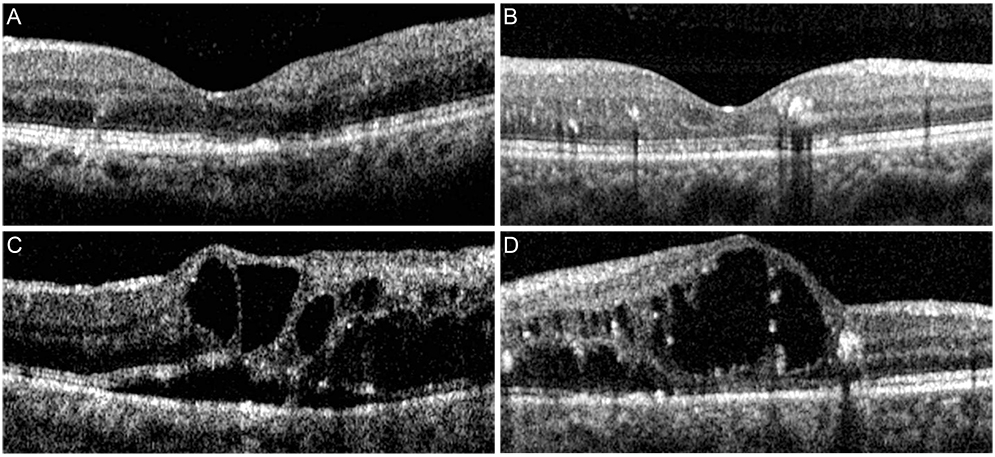
Figure
Reference
-
1. Rogers SL, McIntosh RL, Lim L, et al. Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010; 117:1094–1101.2. McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010; 117:1113–1123.3. Campochiaro PA, Hafiz G, Shah SM, et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008; 16:791–799.4. Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1124–1133.5. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1102–1112.6. Shin HY, Jee DH. The short-term efficacy of intravitreal ranibizumab for macular edema in central retinal vein occlusion. J Korean Ophthalmol Soc. 2011; 52:1048–1054.7. Kim JY, Park SP. Comparison between intravitreal bevacizumab and triamcinolone for macular edema secondary to branch retinal vein occlusion. Korean J Ophthalmol. 2009; 23:259–265.8. Chen SD, Sundaram V, Lochhead J, Patel CK. Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006; 141:876–883.9. Gregori NZ, Rosenfeld PJ, Puliafito CA, et al. One-year safety and efficacy of intravitreal triamcinolone acetonide for the management of macular edema secondary to central retinal vein occlusion. Retina. 2006; 26:889–895.10. Oh JY, Seo JH, Ahn JK, et al. Early versus late intravitreal triamcinolone acetonide for macular edema associated with branch retinal vein occlusion. Korean J Ophthalmol. 2007; 21:18–20.11. Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010; 117:1134–1146.12. Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol. 2009; 127:1115–1128.13. Ip MS, Scott IU, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 5. Arch Ophthalmol. 2009; 127:1101–1114.14. Fine SL. Early detection of extrafoveal neovascular membranes by daily central field evaluation. Ophthalmology. 1985; 92:603–609.15. Yang CS, Cheng CY, Lee FL, et al. Quantitative assessment of retinal thickness in diabetic patients with and without clinically significant macular edema using optical coherence tomography. Acta Ophthalmol Scand. 2001; 79:266–270.16. Schaudig UH, Glaefke C, Scholz F, Richard G. Optical coherence tomography for retinal thickness measurement in diabetic patients without clinically significant macular edema. Ophthalmic Surg Lasers. 2000; 31:182–186.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laser Photocoagulation for Macular Edema in Branch Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema
- Visual Prognosis of Macular Edema Associated with Macular Ischemia in Branch Retinal Vein Occlusion
- Clinical Aspect of Branch Retinal Vein Occlusion
- The Effect of Laser Treatment on Branch Retinal Vein Occlusion